CHAPTER 13
Intercourse Difficulties In Women:
Pain, Discomfort, And Fear
Female dyspareunia . . . may be one of the
earliest recognized sexual dysfunctions . . . the most
common . . . possibly the most underreported
. . . and the sexual dysfunction most linked to physiological
pathology. Perhaps one of the reasons why the
literature . . . is filled with absolutes is
because of one further distinction - it is
clearly the most underinvestigated . . .
Meana and Binik, 19941
The Problem
A 32-year-old nurse was seen in
consultation with her 35-year-old husband. They
were married seven years and had two
children. Their sexual experiences had always
been pleasurable and free of problems until
two years ago. Immediately after the
birth of their second child, she
experienced persistent pain whenever intercourse
was attempted. The pain was located at the
entrance to her vagina and became evident
only with entry. Before her vaginal pain
began, the frequency of intercourse was
several times each week but now was reduced
to once or twice each month. She and
her husband remained sexually interested
and sexual activity (excluding, by agreement,
attempts at intercourse) occurred several
times each week.
The use of tampons had never been a source
of difficulty for her but she stopped
using them after her last childbirth.
Vaginal examinations by her doctor were uncomfortable
in the past but now they were associated with
great pain. At her request her
husband stopped inserting his finger into
her vagina during sexual experiences. On
examination by a gynecologist, there was
vaginal spasm at the introitus and mild
reddening in the 4 to 9 o’clock area of the
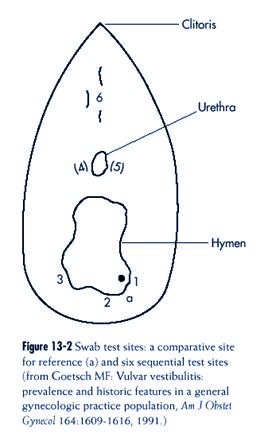
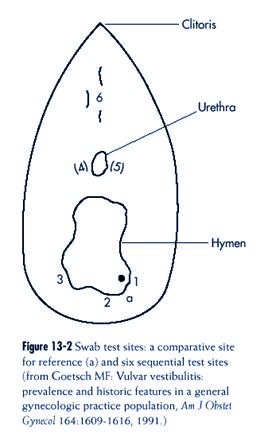
vestibule. The cotton swab test (see Figure
13-2 and `Physical Examination’ below in
this Chapter) showed exquisite tenderness
in this same region, indicating a diagnosis
of vulvar vestibulitis.
Anesthetic ointment relieved her pain
temporarily but also diminished pleasurable
feelings. Vaginal dilators helped relieve
the vaginal spasm so that when intercourse
occurred it was less painful. Surgery was
discussed with her and while she
and her husband viewed this as a possible
option, they preferred to wait until other
approaches were exhausted.
A 23-year-old school teacher was seen with
her husband of eight months because
intercourse was attempted on many occasions
but had never actually occurred
(either during her marriage or before). She
reported experiencing vaginal discomfort
when intercourse was attempted. Both were born of families that emigrated
from Asia and had known each other since
childhood. The marriage was born of a
love relationship rather than having been
arranged but they nevertheless refrained
from including intercourse in their sexual
activities before their wedding because of
family, religious, and cultural
proscriptions. Both families were applying not-sosubtle
pressure on the couple to have children. No
one else knew of their inability
to have intercourse. She was terrified of
pain and expected to experience pain with
anything entering her vagina (or going out,
hence also her fear of childbirth). Her
dread of pain with intercourse was so
strong that she cried out when he neared her
vulva (a reaction that made him
progressively less enthused about making any
attempt at vaginal entry).
In an initial inspection-oriented pelvic
examination, the patient was in a semireclining
position and watched the procedure with a
handheld mirror. Cotton swab
test was negative. When on a subsequent
occasion the end of the physician’s finger
was introduced into the patient’s vagina,
the physician could feel a ring of surrounding
muscle. The diagnosis of vaginismus was
made and the patient and her
husband began a treatment program. About
four months later, intercourse occurred
successfully on many occasions, and when
last seen she was pregnant.
Terminology
Terminology problems have more to do with
health professionals than with patients
or the lay public. Vulvodynia is a
general term recommended by the International
Society for the Study of Vulvar Disease
(ISSVD) to describe any chronic discomfort
or pain in the vulvar region regardless of
etiology and not necessarily related to
sexual activity.2 Dyspareunia
is
more specific in describing pain associated with sexual
intercourse. Dyspareunia could be felt at the
point of vaginal entry, associated with
the back and forth movements of intercourse,
or deep within the patient’s vagina.
Insofar as pain with intercourse is
discussed, this chapter concerns itself principally
with the first.
However, patients may complain of vaginal
“discomfort,” rather than pain, when
intercourse occurs. Whether such discomfort
always represents mild pain, does so
sometimes, or is something else altogether is
unclear. The multiplicity of problems
that are inherent in the present use of the
word “dyspareunia” were outlined by
Meana and Binik and include issues such as
unclear definition, disagreement over
the inclusion or exclusion of certain
disorders (such as vaginismus and postmenopausal
vaginal dryness), confusion about the role of
physical and psychological factors
in the etiology, and the meaning of not
finding abnormalities on pelvic examination.
1 Another source of confusion can be found in
the use of the word vaginismus,
which in the literature describes (1) a
physical sign accompanying various casuses
of painful intercourse and (2) a specific
disorder. (In this Chapter, the words “vaginal
spasm” will be used to describe the former,
and “vaginismus” will refer to the
latter).
Vulvar vestibulitis (VVS) is a
specific diagnostic term that is defined and discussed
below in this chapter.
Classification
While the heading “Sexual Pain Disorders” was
not carried over from DSM-IV3 to
DSM-IV-PC4, both
classification systems continue a tradition of asking clinicians to
think of two disorders (dyspareunia and
vaginismus), and to do so in an either/or fashion.
The criteria for both are summarized in the
PC version respectively as follows:
“recurrent or persistent genital pain . . .
before, during, or after sexual intercourse,
causing marked distress or interpersonal
difficulty” (p. 117) and “recurrent or persistent
involuntary spasm of the musculature of the
outer third of the vagina that interferes
with sexual intercourse, causing marked
distress or interpersonal difficulty” (p. 118).4
Classification Problems: Distinguishing Dyspareunia
And Vaginismus
In relation to the problem of pain,
discomfort, and/or fear of intercourse in women,
DSM-IV-PC4 definitions
and accompanying clinical information often conflict with
clinical experience and result in confusion
when trying to distinguish dyspareunia and
vaginismus. The two often occur together. For
example, when intercourse is attempted
in the context of vaginismus, patients
usually complain of pain (although fear of pain
may be much more prominent). Likewise, when
persistent painful intercourse occurs
for reasons other than vaginismus, it is
clinically commonplace to see associated vaginal
spasm. In such instances, vaginal spasm
seemingly functions as a symptomatic and
defensive (usually involuntary) reaction of
the woman to protect herself against anticipated
pain.
Subclassification: Descriptions
Theoretically, the subclassification of
disorders that cause fear, discomfort, or painrelated
difficulties with intercourse in women
involve the assessment of whether the
problem is lifelong or acquired, situational
or generalized. In clinical practice, the first
two patterns described below are most
commonly seen; the third probably occurs
frequently in the community but is uncommonly
presented to health professionals.
The assessment of pain, discomfort, or fear
associated with attempts at intercourse in
women is outlined in Figure 13-1.
Lifelong and Generalized
When hearing that pain or fear associated
with attempts at intercourse have always
existed, the history is often that of an
unconsummated marriage. Not only has a man’s
penis never entered her vagina, but the same
story is also heard concerning her own,
or her partner’s fingers, tampons or a
physician’s fingers or speculum. Alternatively,
vaginal entry of a current or previous
partner’s penis may have taken place but pain
persisted through much of the experience of
intercourse. Prior to intercourse attempts
(e.g., in the premarital period when a woman
resolutely decides against having intercourse
before marriage), she often found herself
sexually interested, wet, and possibly
orgasmic. While this response may have
continued in the short run (e.g., after marriage),
the pattern may have altered in the long run
as a result of pain and fear connected
to present attempts at penile entry. In such
a situation, women typically feel
self-deprecatory, saying that they feel
“abnormal” as women and as a marital and sexual
partner. In a frenzy of ambivalence, she may
have explicitly suggested to her partner
that he “find himself someone else” while
simultaneously fearful that he will do exactly
that. The agony of feeling unable to become
pregnant through intercourse is often the
final straw that drives her to the
humiliating admission that help is necessary to accomplish
what television, magazines, and billboards
shout is a common event for the rest
of mankind.
A 22-year-old woman saw her family doctor
because she had married three weeks
before but was unable to have intercourse
despite numerous attempts. It was evident
that she was fearful of vaginal entry but
it was not evident whether she also
experienced pain when intercourse was
attempted. She and her husband were sexually
active with one another in the three years
of their courtship but decided for
religious reasons that intercourse should
be included only after they married. Their
sexual practices did not include vaginal
insertion of his fingers, and, as well, she
never had intercourse with a previous
sexual partner, did not like the idea of tampons,
and never had a vaginal examination from a
physician. Neither she nor her
husband described any other difficulties
with their sexual function.
A pelvic examination was scheduled for the
following day when the physician
could allocate a greater amount of time.
The external vulvar examination revealed
no structural pathology and a negative swab
test. The physician then explained her
diagnostic impression of vaginismus and
aspects of the anatomy and physiology of
the patient’s vagina, reassured the patient
that there were no apparent structural
problems impeding intercourse, described
the importance of control by the patient
in relation to vaginal insertion, and
encouraged the patient to insert her own and
then the doctor’s finger part-way into her
vagina. With patience and encouragement
from the doctor, finger insertion took
place. The patient was enormously
pleased and felt a sense of accomplishment.
She was encouraged to guide her husband’s
penis into her vagina in the same manner as
her own finger. When seen one
week later, the patient related that
intercourse occurred on three occasions, the
last two times without any difficulty.
A 38-year-old woman was seen alone because
of a lifelong inability to have intercourse.
Her first marriage was annulled after five
years, primarily because of “nonconsummation.”
She had pleasurable sexual experiences
since her separation ten
years before but she always managed to
avoid attempts at intercourse. Over the
years, she was unwilling to accept
suggestions made by her family physician (aware
of the problem because of the impossibility
of vaginal examinations) for referral to
a sex therapist. Presently, she was in the
midst of a serious relationship and was
contemplating marriage. However, she was
also fearful of the implications of her
inability to engage in intercourse. Her
partner was accepting of this limitation but
at the same time was encouraging her to
obtain medical care.
A vaginal examination, conducted by a
consultant, resulted in a negative swab
test, and it was possible to only partially
insert a single finger because of enormous
fear of pain and severe muscular tightness
at the vaginal entrance. A suspected
diagnosis of vaginismus was confirmed. She
remained unwilling to consult
a sex therapist and insisted on not
involving her partner in the treatment program,
explaining that she had this problem long
before their relationship began.
She was unable to insert the smallest
dilator and felt pessimistic about the benefit
of this approach. When last seen she had
remarried and was sexually active without
intercourse.
Acquired and Generalized
In this syndrome, the most commonly heard
story concerning vaginal pain with intercourse
is that the woman had no prior difficulty.
Typically, her previous sexual enthusiasm,
ease of arousal, and orgasm contrasts sharply
with her present reticence. The
current experience of pain tends to be
associated with anything entering her vagina
(penis, fingers, a vaginal speculum), and the
discomfort is particularly located at the
vaginal entrance and especially in the
“horseshoe” 4 to 8 o’clock area. The intercourse
pain is described as “tearing” and occurs
with initial vaginal entry but is sometimes
characterized as burning and connected more
with the friction of continuous coital
movement. Discomfort may continue for several
hours after the sexual experience.
A 27-year-old woman, married four years,
was seen by her family physician because
of pain associated with intercourse. She
related that before the past two years, she
only rarely experienced pain during
intercourse and it lasted only a matter of seconds
and was relieved by change in position. Her
sexual interest was equal to that
of her husband and other male partners
before she married, she had no difficulty
becoming vaginally wet when interested, and
would easily come to orgasm. Since
the past two years, all of this had
changed. Pain associated with vaginal entry had
become gradually more common and
increasingly severe and as a result she found
herself only marginally interested in
sexual activities, often used an artificial lubricant
because of insufficient vaginal
lubrication, and only occasionally would come
to orgasm. She described the pain as in the
6 o’clock area of her introitus, burning
in character, and somewhat relieved by the
cessation of intercourse, although the
discomfort after would necessitate her
sitting in a bath to obtain some lessening of
the feeling of irritation.
On examination, the swab test was positive
in many locations and a diagnosis
of vulvar vestibulitis (VVS) was made. With
an initial focus on her diminished
sexual desire, psychologically oriented
treatment was begun. Counseling also
focused on helping her and her husband
explore other sexual practices other than
intercourse. Intercourse occurred
periodically and was eventually experienced with
little or no discomfort on her part.
Despite improvement on many levels, her lack
of sexual enthusiasm did not change and
more aggressive treatment of her VVS at
that time was not something she thought
desirable.
Acquired and Situational
In contrast to the lifelong form, the history
reveals intercourse without difficulty in the
past, and in contrast to the generalized
form, only vaginal entry of a man’s penis in the
present results in discomfort (rather than
tampons, fingers, and speculum). Other features
of the syndrome may include the following:
• Variability in appearance of the pain, age
of patient (youth), sexual
inexperience
• The presence of psychosocial explanatory factors
• The lack of pathological findings with
pelvic examination
None of these features are pathognomonic.
A 19-year-old single woman was concerned
that since about six months ago, intercourse
was associated with pain—a facet of her
sexual experiences that had never
occurred before in previous relationships.
Although dyspareunia was frequent now,
it was also quite irregular. Her
relationship with her boyfriend of ten months was
frequently stormy, and on two occasions
they decided to stop dating. She was still
unsure about continuing the relationship
and had not told him of her sexual discomfort.
She had no difficulty using tampons now or
in the past during her menstrual
periods, and likewise, experienced no
problems with pelvic examinations by
a physician. The pain that she experienced
was not localized, would arise only with
vaginal entry, and disappeared when his
penis left her vagina. Pelvic examination
revealed no structural pathology and the
swab test was negative. When seen three
months later, she had begun a relationship
with another man with whom she was
in love and found that her dyspareunia had
disappeared.
Epidemiology
In the general population study conducted by
Laumann and his colleagues, respondents
were asked the following question: “During
the last 12 months, has there ever been a
period of several months or more when you
experienced physical pain during intercourse?”
5 (p.371) Overall, this was answered with a
“yes” by 14% of the women (in
contrast to 3% of the men). The age group in
which this was most commonly reported
was 18 to 24 (22%) and was least commonly
reported in those over 50 (7% to 9%). As
with other sexual problems, pain with
intercourse was positively correlated with the
respondent’s health status (p. 373) (9% of
women who’s health status was “excellent”
compared to 23% of those in “fair” health).
There was also a positive
correlation with “happiness” (p. 374) in that
pain with intercourse was
reported by 12% of those who were “extremely
happy” versus 28% of
those who were “unhappy most times.” While
intercourse pain is obviously
common among women in the general population,
vaginismus as
a specific disorder seems unusual. Subtypes
of pain associated with intercourse,
and the subject of unconsummated marriages,
were not addressed
in the Laumann5 or Kinsey6,7 studies.
When asked the question: “During the
last 12 months has there ever been a
period of several months or more when
you experienced physical pain with
intercourse?”5 14%
of the women
answered “yes.”
|
Meana et al. completed a descriptive study of
a nonclinical sample of 112 women
recruited by newspaper advertisement and
ranging in age from 19 to 658 with pain
relating to intercourse. Subjects underwent
thorough psychological and gynecological
examinations. The subjects were eventually
grouped under four diagnostic subheadings:
• The largest (46%) were diagnosed as having
vulvar vestibulitis
• The next largest (24%) had no
dyspareunia-related physical findings
• The third (17%) was “mixed” (described by
the authors as a “catchall”)
• The fourth (13%) was the vulvar/vaginal
atrophy group
Apart from community studies, Goetsch
provided information on the prevalence of
dyspareunia and vulvar vestibulitis in an
unreplicated study of a general gynecology
practice.9 All
patients (n = 10) seen by her in a six month period were questioned and
their examination included a swab test.
Twenty percent described symptoms of pain
and all except three had a positive swab
test. Thirty-one patients (15% of the entire
group) were diagnosed as having vulvar
vestibulitis. Affected patients were typically
premenopausal.
Information about the epidemiology of
vulvar/vaginal atrophy (typically found in
postmenopausal women) and its consequences
was assessed in a general population
study conducted in Sweden on a random sample
of 5990 women ranging in age from
46 to 62 (five birth cohorts).10 Subjects
were sent a questionnaire (response rate 76%)
that included questions on various
climacteric symptoms. Vaginal dryness was reported
by 21% overall and showed a linear increase
(4% to 34%) in each cohort. In spite of
lubrication difficulty, approximately 60% had
a “regular sex-life” and only 8% of the
entire sample reported that vaginal dryness
was the reason for the absence of sexual
activity (although 32% of the 62-year-old
women said so).11
It
is instructive to note
that in another study which involved the
transition to menopause, one third of premenopausal
women reported vaginal dryness, thus
indicating that factors other than
hormones can have a major influence on
vaginal lubrication.12 In addition, a study of
48 postmenopausal women that included
psychophysiological measurements supported
the notion that vaginal dryness in
postmenopausal women might well be related to
nonhormonal sexual arousal problems.13
In a review of the incidence and prevalence
of sexual dysfunctions in “sex clinics,“
vaginismus was found to vary from 12% to 17%
“of the females presenting with problems
in sexual dysfunction clinics . . .
reflecting a rather stable rate.”14 In the same
review, dyspareunia rates were estimated at
3% to 5% but the authors wondered if this
complaint was more often made to family
physicians and gynecologists than sex therapists.
Support for this was given by the Laumann
data5, and, as
well, a survey of
physicians15 who
reported that “dyspareunia, or painful intercourse” was the sixth most
common sexual problem seen out of a list of
20 items.
Etiology
Entry dyspareunia that lasts for a short
period of time (days to weeks) is probably common
and may result from vaginal irritation as a
consequence of infection or allergy.
Although there are many explanations for more
persistent entry dyspareunia,16 three
problems probably account for most cases of
pain, discomfort, or fear of intercourse in
women:
• Vulvar vestibulitis
• Postmenopausal vulvar/vaginal atrophy and
consequent vaginal
dryness
• Vaginismus
Vulvar Vestibulitis
Friedrich17 coined the
term vulvar vestibulitis (VVS) and described three
criteria for the diagnosis:
1. Severe pain on vestibular touch or
attempted vaginal entry
2. Tenderness to pressure localized within
the vulvar vestibule
3. Physical findings confined to vestibular
erythema of varying degrees
Women with VVS are typically in their 20s and
30s and of Caucasian origin. Goetsch
(see Epidemiology above) provided details of
her 31 subjects (plus seven who were
diagnosed with VVS before the beginning of
her six month study).9 The median length
of the complaint was 8.5 years and half of
the respondents first noted pain with tampon
use rather than with sexual intercourse. Half
of the women always had pain dating
from the first attempt at intercourse (often
designated as “primary”). A significant subgroup
(21%) experienced dyspareunia in the
postpartum period, and delivery by cesarean
section made no difference in its appearance.
The etiology of VVS is unknown, giving rise
to several theories.17-19 Infectious agents
have received much attention. Some observers
note a high rate of repeated vaginal and/
or urinary tract infections (such as
candidiasis). Human papillomavirus (HPV) is also
suspected. A majority of Goetsch’s patients
had no known association with HPV. However,
“unusually large doses of fluorouracil cream
. . . had caused severe chemical
burns in two patients and evolved into the
most severe cases of vestibulitis seen in the
survey.”9 “The only
infectious agent found to directly cause or worsen vestibulitis was
group B streptococcus” in two patients.9 Eighty
percent of patients in the Goetsch study
who always had pain and who had sisters knew
of a female relative with dyspareunia or
intolerance of tampons. There was no such
association in those whose
pain began later. Investigators into the
psychological status of patients
with dyspareunia generally found evidence of
more symptoms than nopain
matched controls.8 However,
no differences were found when
those who specifically had VVS were separated
from other subtypes.
Goetsch concluded that swab testing
demonstrated a continum
from those who were positive but had no
clinical pain to those who
were dysfunctional.9 Likewise,
she indicated that when pain was present,
it was “minor for many, and accommodation was
aided even by
getting an explanation of the problem.”9 Last, she
noted that many had
sensitivity that predated sexual
exposure.
Three problems probably account for
most cases of pain, discomfort, or fear
of intercourse in women:
• Vulvar vestibulitis
• Postmenopausal vulvar/vaginal atrophy
and consequent vaginal dryness
• Vaginismus
Goetsch concluded that swab testing
demonstrated a continuum from those
who were positive but had no clinical
pain to those who were dysfunctional.9
Likewise, she indicated that when pain
was present, it was “minor for many,
and accommodation was aided even by
getting an explanation of the problem.”9
|
Postmenopausal Vulvar/Vaginal Atrophy
Vaginal lubrication largely depends on
estrogen stimulation of the vaginal mucosa and,
therefore, vaginal dryness is usually
considered to be associated with
the diminution of estrogen that accompanies
menopause. Atrophic
alterations occur to the vaginal epithelium
in the absence of estrogen
and are associated with increased vaginal pH,
decreased vaginal fluid,
and decreased vaginal blood flow.20 Exogenous
estrogens appear to
reverse these changes. However, a woman’s
level of sexual activity
(including masturbation) and her circulating
androgens have also been
demonstrated to influence the extent of
vaginal atrophy.21 While vaginal atrophy and
dryness is often reported as uncomfortable,
the extent to which actual pain is experienced
during intercourse is unclear.
Vaginismus
Vaginismus represents an involuntary spasm of
the muscles surrounding the outer third
of the vagina, resulting in narrowing of the
vaginal entrance and inability or difficulty
in allowing vaginal entry in the waking
state. The sex-related result of vaginismus is
the inability to engage in intercourse
(either at all or without significant discomfort).
The history is usually lifelong (that is,
since the patient tried to put anything into her
vagina) but not all such lifelong histories represent
this disorder. A similar story may
be given in some instances of vulvar
vestibulitis (see Vulvar Vestibulitis above).9
Patients give various explanations for
vaginismus including22:
1. Thinking sexual activity to be sinful or
offensive
2. Fear of pregnancy or childbirth
3. Lack of anatomical awareness
4. Homoerotic feelings
5. Dislike of semen
6. Aversion to a man’s penis or men in
general
Some specialists view such phenomena as
symptoms rather than
causes.23 As
counterintuitive as it might seem, a history of genital
trauma or sexual violence in the histories of
women with vaginismus is
unusual.24 When
patients were asked their opinions about possible
causes, they placed fear of pain and fear of
intimacy high on the list.25
Patients may describe pain with intercourse
attempts but fear of vaginal
entry rather than the actual experience of
pain may be the principal
factor that interferes with intercourse.
Other sexual difficulties (e.g., a desire disorder)
may be present in the patient and may have antedated
awareness of intercourse trouble.
Investigation
History
History is only one element, albeit an
essential one, in defining fear, discomfort, or
pain in women associated with intercourse
attempts, and in many instances, helping to
delineate the cause. Issues to inquire about
and suggested questions include:
While vaginal atrophy and dryness is
often reported as uncomfortable, the
extent to which actual pain is experienced
during intercourse is unclear.
When patients were asked for possible
causes of vaginismus, they placed pain
and fear of intimacy high on the list.
Patients may describe pain with intercourse
attempts but fear of vaginal
entry rather than the actual experience
of pain may be the principal factor that
interferes with intercourse.
|
1. Duration (see Chapter 4, “lifelong versus
acquired”)
Suggested Question: “How long has this
been a problem for you?”
Alternative Suggested Question if Intercourse
Occurred in the Past: “Have you even
been able to have intercourse without
experiencing pain?”
2. Intravaginal experience in the past (see
Chapter 4, “generalized versus situational”)
Suggested Question: “What has been your
experience with tampons?”
Suggested Question: “What has been your
experience with inserting
your own finger into your vagina?”
Suggested Question: “What has been your
experience with a sexual
partner inserting a finger into your vagina?”
Suggested Question: “What has been your
experience with doctors
performing a pelvic examination and using
fingers or a speculum?”
Suggested Question: What has been your
experience with wearing
tight clothes such as jeans?
3. Intravaginal experience in the present
(see Chapter 4, “generalized versus situational”)
Suggested Question: “What is it like for
you now when a sexual
partner attempts to insert his penis (or his
finger) into your
vagina?”
Additional Suggested Question: “Does it
matter if you are with a different
sexual partner?”
4. Location of the pain (see Chapter 4,
“description”)
Suggested Question if Intercourse Occurs: “Where
do you actually feel
the pain? At the entrance? Within your vagina
during intercourse?
Or deep inside?”
Additional Suggested Question for Entry Pain:
“If you were to compare
the opening to your vagina to a clock, at
which point on
the clock do you feel pain?”
Additional Suggested Question to Determine if
Pain is Associated with Thrusting: “Is
the pain felt on the inside of your vagina as
he is moving in
and out?”
Additional Suggested Question to Determine if
the Pain is Deep: “When he
inserts his penis deeply, does it feel as
though he is poking
something?”
5. Character of the pain (see Chapter 4,
“description”)
Suggested Question: “Sometimes a person
experiences fear of intercourse
more than actual pain. Does this ever happen
to
you?”
Additional Suggested Question if Intercourse
Occurs: “What does the pain
feel like? For example, does it feel as
though it is tearing or
burning?”
6. Factors that result in improvement or
worsening (see Chapter 4, “description”)
Suggested Question: “Is there anything
that makes the
pain better?”
Additional Suggested Question: “Is there
anything that
makes the pain worse?”
Additional Suggested Question if Intercourse
Occurs: “What does
it feel like when he ejaculates?”
Physical Examination
Any complaint of persistent pain associated
with vaginal entry requires
a complete physical examination, which need
not take place on the
first visit or be completed on one occasion.
For example, in the context
of vaginismus, a vaginal examination might
well be terrifying to the
patient and, as well, impair the
physician-patient relationship. A speculum
examination under such circumstances may have
even more severe consequences.
Rafla described a case in which a vaginal
examination in the context of vaginismus
resulted in physical injury and a blood loss
of 1000 ml.26
Considerably
more time (and
patience) is usually required than in a more
“ordinary” pelvic examination (see “Physical
Examination” in Chapter 6).
When the patient’s history is one where
intercourse has never occurred because
attempts resulted in pain, discomfort, or
fear, it is reasonable to engage in a preparatory
process before an actual intravaginal
examination.27
The
patient touches herself as
close to the introitus as possible, daily, in
private, and for five to ten minutes. While
this is taking place, she is asked to imagine
herself being examined, view her genitalia
with a mirror, and is shown how to insert her
own fingertip around the anterior vaginal
Any complaint of persistent pain associated
with vaginal entry requires a complete
physical examination, which need
not take place on the first visit or be
completed on one occasion.
Considerabily more time (and patience)
is usually required for a pelvic
examination
involving persisitent pain associated
with vaginal entry than is required in a
more “ordinary” pelvic examintion.
|
wall using diagrams or models. This
preparation is meant to convey to the patient that
she will be in control of the examination
when it does occur.
The actual pelvic examination in such a
patient begins with an inspection of the
external genitalia. In the syndrome of vulvar
vestibulitis, inspection may reveal varying
degrees of erythema of the vestibular mucosa.17 On this
first occasion, there is no
necessary reason to extend the examination
beyond inspection and explanation. However,
if the patient permits, the examiner can also
gently probe the
vestibular openings to major and minor gland
ducts (the “swab test”)
with a sterile water-moistened cotton-tipped
applicator, to exclude the
possibility of vulvar vestibulitis (Figure
13-2). (The vestibule is bordered
medially by the hymenal ring, laterally by
Hart’s line, anteriorly
by the frenulum of the clitoris, and
posteriorly by the fourchette. The
area contains opening of major [Bartholin’s,
Skene’s, and periurethral]
and minor vestibular glands.)28
When the swab test is positive, colposcopy
might be “helpful in identifying discrete
lesions, which [are] often difficult to see
without aceto-white staining and
magnification”.18
When the swab test is negative, examination
of the interior of the vagina might then
take place. One method of allowing the
patient control over this part of the examination
is to have her hold the physician’s wrist
while she slowly introduces one of the examiner’s
fingers into her vagina. This process may
extend over several visits. Speculum and
Speculum and bimanual examination of
the patient with a history of lifelong
vaginismus should be delayed (barring
some urgent reason) until a later time
when vaginal entry is no longer associated
with pain, discomfort, or fear.
|
bimanual examination of the patient with a
history of lifelong vaginismus should be
delayed (barring some urgent reason) until a
later time when vaginal entry is no longer
associated with pain, discomfort, or fear.
Valins provided a vivid and poignant
first-person account of the pelvic/vaginal
examination of a woman with vaginismus with a
description of how her gynecologist
approached the examination29 (pp.
203-210).
Laboratory Examination
When vaginal infection is considered, several
tests can be done to eliminate the possible
presence of various pathogens. In addition,
biopsy of the vulvar epithelium on
a patient with suspected vulvar vestibulitis
often shows evidence of chronic inflammation.
However, the normal histology of this
area has not been well described. In a
comparison of tissues obtained by punch
biopsy done on women with VVS and normal
controls, both showed evidence of
inflammation, thereby casting doubt on the
value of finding evidence of inflammation on
histological examination of vulvar epithelial
tissue.30
Treatment
Lifelong and Generalized
Most women who have the lifelong and
generalized form of vaginal pain or fear to the
extent that intercourse has never occurred
will likely be diagnosed as having vaginismus
(although some will have primary vulvar
vestibulitis [see below]). Drenth suggest
that when considering the treatment of
vaginismus, couples should separate the issues
of wanting to overcome the intercourse
difficulty from wanting to become pregnant,
decide which is of higher priority, and focus
on that goal.31
In
any
instance, primary care treatment may be
sufficient.
Both partners should be involved in
treatment, although the apparent
passivity of many husbands of women with
vaginismus (noted by
many authors) may contribute to his
relatively small contribution.32
(p. 34). On an impressionistic basis, many
women with vaginismus
seem to have difficulty talking about their
thoughts and feelings,
which in turn makes insight-oriented
psychotherapy with them difficult.
With couples where the man is passive and the
woman unexpressive,
visits are often brief and the focus is on
progress using
dilators and other functional aspects of
their care.
When the diagnosis is vaginismus and
pregnancy is the principal
objective, Drenth suggests artificial
insemination using (1) the husband’s
semen (AIH) and (2) the insemination
procedure performed
by the couple themselves.33 When
overcoming the fear/pain associated
with attempts at intercourse is the principal
objective, couples
are initially advised to stop attempting to
insert the man’s penis into
the woman’s vagina (or anything else such as
his finger), and even to
not consider any form of vaginal entry even
if the circumstances
seem favorable. (Emphasis on thoughts are
crucial, since it is the
When overcoming the fear or pain associated
with attempts at intercourse is the
principal objective, couples are initially
advised to stop any form of vaginal
insertion even if the circumstances seem
favorable. (Emphasis on thoughts are
crucial, since it is the anticipation that
leads to worry.)
The word “dilator” is a misnomer when
used in the treatment of vaginismus
since dilatation does not occur and in
any case is not the purpose of the
procedure.
The problem is not with the
structure of the muscle surrounding the
vaginal opening but rather with its
function.
|
anticipation that leads to worry.) At the
same time, they are encouraged to continue
enjoying the sexual activities other than
intercourse that previously occurred.
After the diagnosis of vaginismus is
confirmed and VVS excluded, as well as insufficient
knowledge of sex-related anatomy and
physiology, vaginal dilator use could be
considered. (Flesh-colored, silicone dilator
sets of four are available at 1-800-621-1278
through Milex Products, 5915 Northwest
Highway, Chicago, ILL 60631). Although
recommended decades ago for this same
purpose, vaginal dilators have become a
therapeutic mainstay since they were
suggested by Masters and Johnson in 1970.34
The word “dilator” is a misnomer when used in
the treatment of vaginismus since
dilatation does not occur and in any case is
not the purpose of the procedure. The
problem is not with the structure of the
muscle surrounding the vaginal opening but
rather with its function. A “dilator” works
rather as an “accommodator” in providing
an opportunity for the woman to become used
to having something in her vagina
without fear or pain, and entirely in her
control.
Supervision of dilator use through the
progressively larger sizes in a set can be readily
undertaken in a primary care setting.
Insertion of dilators should occur daily for the
longest period of time that the patient can
manage, and when she is alone so that the
process remains entirely under her control
(rather than at the urging of her partner).
The largest dilator in the set that does not also
cause discomfort should initially be
used. Liberal amounts of over-the-counter
water-soluble jelly (e.g., K-Y Jelly) should
be applied to the dilator. Progression to the
next size should only take place when
there is complete absence of discomfort with
the size currently used. Eventually, when
she is comfortable with a size that
approximates her partner’s erect penis, she should
be instructed to insert his penis almost as
if it were another dilator. Since intromission
by the woman is accomplished relatively
easily when she is in the superior position,
the couple should practice using that
position before penile insertion is actually
attempted.
If this appears to be a mechanical approach,
it probably is a correct perception, but
only from the health professional’s
viewpoint. Much more than mechanical manipulations
are taking place from the couple’s
perspective. While hope extends backward to
the time the physician’s finger was first
inserted into the patient’s vagina, only her
actual experience of painless penile
insertion represents concrete evidence of change.
Paradoxically though, patients tend to be
more subdued when describing the first
occasion of intromission than is the treating
health professional. The explanation
might be an absence of confidence that the
remainder of the therapeutic tasks can be
successfully completed. However, it is well
to remember at this point that penile insertion
may not be immediately translated into
feelings of pleasure for either person. This
depends on the extent of sexual freedom that
the couple enjoyed before. Some couples
absorb the newly found sexual skills quickly
and zealously. In other instances, pleasure
for the women may take place in an
evolutionary way, extending over a period of time
and in the context of the confidence that is
linked with not having to think about the
placement of body parts. Confidence in that
circumstance tends to occur with repeated
successful experiences.
Most observers use intercourse (consummation)
as the sole criterion for success in
the treatment of vaginismus. Masters and
Johnson describe excellent treatment results
(100%) in their five-year follow-up.34 Van de
Wiel et al. conducted a meta-analysis on
treatment results involving 20 surveys and 17
case studies published between 1960 and
1990.35 They
conclude that several treatment approaches appear to be equally effective
(except surgery, which was not a subject of a
published report) and that the average
rate of success was about 80%. Some describe
a more modest outcome. Drenth et
al. reports on a questionnaire survey of 57
patients (response rate 86%) diagnosed with
“primary vaginismus.”33 Consummation
occurred in 54% overall. In couples who
wanted to become pregnant, consummation
occurred in 74% compared to 33% who
sought treatment only for the intercourse
difficulty. Problems encountered in the treatment
of vaginismus31 include
the following:
1. Lack of clarity around therapeutic aims
2. Intimacy difficulties on the part of the
woman and consequent unwillingness to
involve her partner
3. The emergence of other fears
Desire for a child may be a stronger
motivating factor for the treatment of vaginismus
than desire for intercourse. The survey by
Drenth et al. also provided information on
obstetrical issues.33 Almost one
half (25) of the patients became pregnant (10 as a
result of artificial insemination and 15
through intercourse). Patients who chose selfinsemination
did so for reasons that include the pressure
of time (resulting from a delay
in seeking treatment) or slow therapeutic
progress. The authors felt that insemination
by a physician represented “unnecessary
medicalization” and, furthermore, might
unduly influence any ambivalence toward
pregnancy experienced by the couple.
When self-insemination (also known as home
insemination or AIH [artificial insemination
by husband] is undertaken, it, may be helpful
for a physician to provide technical
advice to the couple and to review methods of
ovulation detection. Briefly, the
insemination process is as follows*: The man
ejaculates [volume of ejaculate is usually
in the range of 2 to 6 cc] into a clean, dry,
plastic or glass container such as a urine
collection bottle from a medical laboratory.
Regular condoms are undesirable for collecting
semen because they may contain a spermicidal
agent. The semen is kept at
body temperature for about 10 minutes (the
sample is then more liquid) and then is
drawn, with minimal accompanying air, into a
narrow syringe (as small as 1 cc in
instances of severe vaginismus but perhaps as
large as 10 to 12 cc). The syringe is
inserted as deep into the woman’s vagina as
possible and the semen is deposited by
pushing on the plunger. During this process,
the woman’s hips should be slightly elevated
with a pillow and she should remain in this position
for about 20 to 30 minutes.
The same process can be repeated in about 24
hours.
Drenth et al. also reported on 26 deliveries
and found that assisted deliveries were
10% higher in patients with vaginismus than
in their clinic population.33 Reasons
included the presence of vaginismus and the
(older) age of the mother. However, they
concluded that having vaginismus does not, in
itself, require special precautions during
labor and delivery. They also observed that:
however counterintuitive the notion might
be, childbirth does not automatically result
in pain- and fear-free intercourse. “Obviously,
a pushing out movement is experienced quite differently from a pushing-in
movement.”33
*Personal
communication, Stacu Elliott, M.D., Co-director, Vancouver Sperm Retrieval
Clinic, VHHSC,
1998.
Acquired and Generalized
As outlined above (see Etiology in this
chapter), vulvar vestibulitis and vulvar/vaginal
atrophy probably account for the majority of
patients seen with the acquired and generalized
form of dyspareunia. When such disorders are
resistant to definitive treatment
within the health care system, active
involvement of the patient in her own care may
be necessary and beneficial. Membership in
the National Vulvodynia Association
(NVA) may prove useful, especially since the
organization produces an informative and
patient-oriented newsletter. (The NVA can be
reached through its Web site [see
Appendix IV], by telephone at [301] 299-0775,
or by mail at P.O. Box 4491, Silver
Spring, MD 20914-4491)
Vulvar Vestibulitis (VVS)
Bergeron and her colleagues19 reviewed
the treatment of VVS and grouped the existing
studies into three categories:
• Surgical intervention
• Medical management
• Cognitive-behavioral/pain management
therapy
Surgical interventions consist of
vestibulectomy and laser therapy. Vestibulectomy has
been the most investigated VVS treatment and
the one reported as having the best
outcome. Laser treatment is described as
controversial and sometimes associated with
negative consequences. Surgery is usually
undertaken after the failure of medial management.
The surgical procedure is typically described
as a modified perineoplasty,
which is performed as day surgery under
general anesthesia. Surgical success usually
has been measured through a one-time
self-report rating of pain with intercourse, and
rates vary from 43% to 100%, with the
majority more than 60%.19
Schover et al. reports an improved outcome
when surgery is combined with sexual
counseling.18 They
describe an eight-month follow-up study on the evaluation and
treatment of a group of 45 women with VVS.
All were treated by conservative local
excision of the vulvar lesions. One of the
factors that indicated a better outcome included
willingness to engage in initial
psychological evaluation and brief post-operative sexual
counseling. Of 32 such patients, 50% reported
that they were much improved. Other
positive predictors were higher socioeconomic
status and localized (versus diffuse) areas
of pain. The authors hypothesize that women
who could accept that their dyspareunia
and vulvar pain was multifactorial in origin
took an active role in rehabilitative efforts
after surgery, and, as a result experienced a
better outcome. They hypothesize that
patients who could not do so might be poor
surgical candidates.
Medical management of VVS typically involves
the use of topical ointments (including
anesthetics, antifungals, and antibiotics),
systemic medications, and other treatments
such as interferon.19 Topical
anesthetics are of limited value, since their effect is shortterm
and allergic reactions may occur. Nonscented
lubricants are also of short-term
value but do not have adverse effects. Other
topical ointments (antibiotics, antifungals,
antiviral, and corticosteroid creams) are
considered to be ineffective but have not been
carefully studied. Acyclovir (oral),
capsaicin (topical), and calcium citrate tablets have
been reported to be beneficial to some
patients. Alpha interferon is not recommended if
colposcopy or biopsy lesions do not show
evidence of HPV changes.
Pain management of VVS has consisted of
biofeedback, behavior
and sex therapy, cold application, and
acupuncture.19
Some
patients
have found benefit from each of these four
approaches. Since vaginal
spasm (often referred to as vaginismus in the
literature) is often found
during the pelvic examination of a patient
with VVS, some have found
the inclusion of vaginal dilators to be a
treatment adjunct.36
Bergeron et al. compared treatment results
for 78 patients with VVS
who were randomly assigned to surgery
(vestibulectomy), biofeedback,
or sex therapy/pain management.37 Measurements
were made pre- and
post-treatment and at six-month follow-up.
Self-reported coital pain
was significantly improved in all groups from
before and after treatment and from before
to 6 month follow-up. However, the
vestibulectomy group was significantly better than
the sex therapy/pain management group
post-treatment. All groups improved significantly
when the frequency of intercourse was
compared post-treatment to 6 months
later. In summary, patients from all three
groups reported significantly more subjective
improvement from post-treatment to 6 month
follow-up. However, the vestibulectomy
group was significantly better than the sex
therapy/pain control group.
Vulvar/Vaginal Atrophy
Estrogen replacement therapy generally
reverses the vaginal changes associated with
menopause. However, restoration of vaginal
tissue function may require up to 18 to 24
months. The long duration may explain the
reason for continued vaginal dryness and
dyspareunia (if the woman is sexually active)
in spite of hormonal and cytologic return
to premenopausal values.38 However,
only a distinct minority of postmenopausal
women use hormone replacement therapy (HRT).
Reasons include the following:
• Personal preference
• Adverse side effects
• It is contraindicated
In addition, some women find that even with
HRT, there is little urogenital benefit.
Thus local (vaginal) forms of treatment have
been developed to counter vaginal dryness
in women who are not on HRT or who need
supplemental therapy for urogenital
symptoms.
Vaginal creams containing estrogen represent
one example of a local form of treatment.
Since estrogen is absorbed from the vaginal
mucosa, a fact that may limit its
acceptability in some patients, attempts have
also been made to find nonhormonal
agents, or, alternatively, to minimize the
absorption of estrogen.
The estradiol vaginal ring represents a
second local treatment option
for vaginal dryness and other urogenital
consequences of estrogen loss.
The development of the ring is based on the
notion that compared to
the amount of estrogen necessary to reverse
vasomotor symptoms (50
mg/day), the amount of estrogen necessary to
alleviate urogenital atrophy
is much smaller (7 to 10 μg/day).39 The ring
delivers a low dose of
“The ring provides a safe and effective
method of pharmacological therapy for
women who require treatment for symptoms
of urogenital aging.”40
Patients from three groups (vestibulectomy,
biofeedback, and sex therapy/pain
management) reported significantly
more subjective improvement from post
treatment to 6 month follow-up. However,
the vestibulectomy group was significantly
better than the sex therapy/
pain control group.
|
17 β-estradiol directly
to the urogenital tissues and has a low level of systemic absorption.
Bachmann reviewed the results of 11 clinical
trials with the estradiol vaginal
ring.40 She found
that it reversed urogenital atrophy, induced minimal stimulation of
the endometrial lining, had few adverse side
effects, and that a single ring was efficacious
for three months of continuous use. Of the
946 postmenopausal women with
treatments up to 96 weeks, “there were
cytological, physiological, physician rating and
patient reporting of either elimination or
amelioration of urogenital atrophy signs and
symptoms.”40 She
concluded that” the risk/benefit ratio has a clear preference to benefit
with risks being very low. Therefore, the
ring provides a safe and effective method
of pharmacological therapy for women who
require treatment for symptoms of urogenital
aging.”40
A vaginal moisturizer is a third local
treatment option. “Replens” is a nonhormonal
nonsystemic vaginal moisturizing gel that has
a low pH, appears to bind to vaginal
tissue, and is applied three times per week.
Replens is based on a polymer (called polycarbophil),
which becomes saturated with water, diffuses
into vaginal epithelial cells,
and then is sloughed off with epithelial cell
turnover.41
This
substance has been studied
in nonhuman primates41 and
humans.42-44
In
two open-label studies of women, Replens
was compared to a locally applied estrogen
cream and found to be safe and effective.
42,43 In one of the studies, both therapies
exhibited statistically significant increases
in vaginal moisture, vaginal fluid volume,
and vaginal elasticity with a return of the
premenopausal pH state. Replens has also been
compared to a water-soluble lubricating
placebo in a double-blind study of women with
a history of breast cancer and
similarly found to be effective.44
A fourth local treatment form that has been
used for many years is an over-thecounter
lubricating gel (e.g., K-Y Jelly).
Acquired and Situational
Little is known about this syndrome except
from patients who describe the problem
of vaginal discomfort with intercourse in the
past, and who have watched it disappear
with the advent of a new relationship. On the
assumption that the difficulty relates
to interpersonal or intrapersonal
psychosocial conflicts, the most reasonable therapeutic
course of action is (1) reassurance to the
woman about the integrity of her genitalia
and (2) psychotherapy, either individual or
couple-related depending on the
circumstances.
Indications For Referral For Consultation
Or Continuing
Care By A Specialist
1. The evaluation of persistent pain
associated with intercourse should always
include a physical/pelvic examination. Thus,
medical consultation should always
be included when a patient with dyspareunia
has been evaluated only by a nonmedical
health professional.
2. Lifelong vaginismus can often be
successfully treated by primary care health
professionals regardless if the goal is
sexual or reproductive. Consultation with
a physician should take place if the treating
health professional is not a MD
to eliminate the possible coexistence of VVS.
When artificial insemination
(AIH) is desired, the couple should be
referred to a physician for advice and
possible assistance. When treatment that is
aimed at overcoming vaginismus
becomes problematic, the couple should be
referred to a sex therapist for
continuing care.
3. Primary (lifelong) VVS may be amenable to
explanation and brief sexual counseling
within primary care. Consultation with a
gynecologist for the purpose of
confirming the diagnosis may be helpful. The
time and skills of a sex therapist
may be particularly useful when intercourse
has never occurred in the past
because of discomfort, and for patients who
are otherwise experiencing significant
sexual difficulty.
4. Secondary (acquired) VVS varies in the
degree of pain experienced. The greater
the extent of pain and sexual complications,
the more a primary care professional
would want to engage the assistance of other
health professionals such as
gynecologists and sex therapists.
5. When dyspareunia in a postmenopausal woman
persists despite adequate vaginal
lubrication, consultation with a sexual
medicine specialist would be desirable to
consider the possibility of other
contributing factors.
Summary
Penile-vaginal intercourse is sometimes
accompanied in women by persistent pain, discomfort,
or fear. Pain can exist at the point of
entry, or deep in the vagina. This chapter
is concerned with the former. Vulvodynia is
a term that encompasses vulvar pain
regardless of etiology, whereas dyspareunia
is specific to pain that occurs with intercourse.
DSM-IV suggests that “dyspareunia” and
“vaginismus” should be separated.
However, if a clinician considers that
“vaginismus” as described in the literature includes
both the disorder as well as vaginal spasm
occurring in the context of several vaginal
disorders, then in fact, vaginismus and
dyspareunia often occur together and separation
becomes clinically difficult.
In community studies, about 15% of women say
they have experienced pain with
intercourse for a few months during the last
year. When dyspareunia is lifelong and
generalized, the causes are usually
vaginismus (the disorder) or vulvar vestibulitis
(VVS). When acquired and generalized, the
etiology is usually VVS (the most common
cause in premenopausal women) or
vulvar/vaginal atrophy with associated vaginal
dryness (the most common cause in
postmenopausal women). When acquired and
situational, the genesis of dyspareunia is
most often related to interpersonal or intrapersonal
difficulties.
The assessment of persistent vaginal pain
involves a history and a physical/pelvic
examination. The latter should include a swab
test whenever vulvar vestibulitis is considered.
In cases where vaginal entry has never
occurred or where there is severe
introital pain, the pelvic examination may
require more than one visit and a lengthy
period of time to complete.
Early or mild instances of vaginismus may
respond to education and supportive
counseling. Treatment of patients who are not
helped by such an approach depends
heavily on the use of dilators and the
support of the patient’s partner and health care
clinician. Sometimes the couple is primarily
interested in reproduction rather than
solving the intercourse problem. In such an
instance, assisting in the process of artificial
insemination using the husband’s sperm (AIH)
may be most productive.
Vulvar vestibulitis is sometimes amenable to
explanation, but in other instances it
may be difficult to treat. Several medical,
surgical, and sex therapy/cognitive-behavior
therapy methods have been suggested. Surgery
(vestibulectomy) has received the most
attention in the VVS treatment literature and
studies indicate this form of treatment to
provide the best results.
At least five approaches can be used in the
treatment of women with dyspareunia
resulting from vulvar/vaginal atrophy and
associated vaginal dryness: oral hormone
replacement therapy (HRT), estrogen cream,
the estradiol vaginal ring (Estring), a
nonhormonal vaginal moisturizer (“Replens”)
and nonhormonal and nonscented
lubricants.
REFERENCES
1. Meana M, Binik YM: Painful coitus: a review of female
dyspareunia, J Nerv Ment Dis
182:264-272,1994.
2. Paavonen J: Diagnosis and treatment of vulvodynia, Ann
Med 27:175-81, 1995.
3. Diagnostic and statistical manual of mental
disorders, ed 4, Washington, 1994, American
Psychiatric Association.
4. Diagnostic and statistical manual of mental
disorders, ed 4, Primary Care Version, Washington, 1995,
American Psychiatric Association.
5. Laumann EO et al: The social organization of
sexuality: sexual practices in the United States,
Chicago, 1994, The University of Chicago Press.
6. Kinsey AC, Pomeroy WB, Martin CE: Sexual behavior
in the human male, Philadelphia and
London, 1949, W.B.Saunders.
7. Kinsey AC et al: Sexual behavior in the human
female, Philadelphia and London, 1953,
W.B.Saunders.
8. Meana M et al: Dyspareunia: sexual dysfunction or pain
syndrome?, J Nerv Ment Dis
185:561-569, 1997.
9. Goetsch MF: Vulvar vestibulitis: prevalence and
historic features in a general gynecologic
practice, Am J Obstet Gynecol 164:1609-1616, 1991.
10. Stadberg E, Mattsson L-A, Milson I: The prevalence
and severity of climacteric
symptoms and the use of different treatment regimens in a
Swedish population, Acta
Obstet Gynecol Scand 76:442-448,
1997.
11. Stadberg E, Mattsson L-A, Milson I: Womens attitudes
and knowledge and the
climacteric period and its treatment. A Swedish
population-based study, Maturitas
27:109-116, 1997.
12. Larson B, Collins A, Landgren A-M: Urogenital and
vasomotor symptoms in relation to
menopausal status and the use of hormone replacement
therapy (HRT) in healthy
women during the transition to menopause, Maturitas 28:
99-105, 1997.
13. Laan E, van Lunsen RHW: Hormones and sexuality in
postmenopausal women: a
psychophysiological study, J Psychosom Obstet Gynecol 18:126-33,
1997.
14. Spector IP, Carey MP: Incidence and prevalence of the
sexual dysfunctions, Arch Sex
Behav 19:389-408, 1990.
15. Burnap DW, Golden JS: Sexual problems in medical
practice, J Med Educ 47:673-680,
1967.
16. Abarbanel AR: Diagnosis and treatment of coital
discomfort. In LoPiccolo J, LoPiccolo L
(editors): Handbook of sex therapy, New York,
1978, Plenum Press.
17. Friedrich EG: Vulvar vestibulitis syndrome, J
Reprod Med 32:110-4,1987.
18. Schover LR, Youngs DD, Cannata R: Psychosexual
aspects of the evaluation and
management of vulvar vestibulitis, Am J Obstet Gynecol
167:630-636, 1992.
19. Bergeron S et al: Vulvar vestibulitis syndrome: a
critical review, Clin J Pain 13:27-42,
1997.
20. Semmens J, Wagner G: Estrogen deprivation and vaginal
function in postmenopausal
women, JAMA 248:445-448, 1982.
21. Leiblum SR et al: Vaginal atrophy in the
postmenopausal woman: the importance of
sexual activity and hormones, JAMA 249:2195-2198,
1983.
22. Blazer JA: Married virgins: a study of unconsummated
marriages, J Mar Fam 26: 213-214,
1964.
23. Dawkins S, Taylor R: Non-consummation of marriage: a
survey of seventy cases, Lancet
ii:1029-1033,1961.
24. Barnes J: Primary vaginismus (part 2): aetiological
factors, Irish Med J 79:62-65, 1986.
25. Ward E, Ogden J: Experiencing vaginismus: sufferers’
beliefs about causes and effects,
Sexual Marital Ther 9:33-45,
1994
26. Rafla N: Vaginismus and vaginal tears, Am J Obstet
Gynecol 158:1043, 1988.
27. Basson R: Lifelong vaginismus: a clinical study of 60
consecutive cases, Soc Obstet Gynecol
Can 18:551-561, 1996.
28. Marinoff SC, Turner MLC: Vulvar vestibulitis
syndrome: an overview, Am J Obstet Gynecol
165:1228-33, 1991.
29. Valins L: When a woman’s body says no to sex:
understanding and overcoming vaginismus, New York,
1992, Viking Penguin.
30. Lundqvist EN et al: Is vulvar vestibulitis an
inflammatory condition? A comparison of
histological findings in affected and healthy women, Acta
Derm Venereol (Stockh)
77:319-322, 1997.
31. Drenth JJ: Vaginismus and the desire for a child, J
Psychosom Obstet Gynecol 9:125-137, 1988.
32. Friedman LJ: Virgin wives: a study of
unconsummated marriages, London, 1962, Tavistock
Publications.
33. Drenth JJ et al: Connections between primary
vaginismus and procreation: some
observations from clinical practice, J Obstet Gynecol 17:195-201,
1996.
34. Masters WH, Johnson VE: Human sexual inadequacy, Boston,
1970, Little, Brown and
Company.
35. Van de Wiel HBM et al:Treatment of vaginismus: a
review of concepts and treatment
modalities, J Psychosom Obstet Gynecol 11:1-18,
1990.
36. Abramov L, Wolman I, David MP: Vaginismus: an
important factor in the evaluation and
management of vulvar vestibulitis syndrome, Gynecol
Obstet Invest 38:194-197, 1994.
37. Bergeron S et al: A randomized controlled
comparison of vestibulectomy, electromyographic biofeedback,
and group sex therapy/pain
management in the treatment of dyspareunia resulting from vulvar vestibulitis.
Paper presented at the meeting of the Society for Sex
Therapy and Research, Fort
Lauderdale, March, 1998.
38. Semmens JP et al: Effect of estrogen therapy on
vaginal physiology during menopause,
Obstet Gynecol 66:15-18, 1985.
39. Heimer G, Samsioe G: Effects of vaginally delivered
estrogens, Acta Obstet Gynecol Scand
163(Suppl):1-2, 1996.
40. Bachmann G: The estradiol vaginal ring: a study of
existing clinical data, Maturitas
22(Suppl):S21-S29, 1995.
41. Hubbard GB et al: Evaluation of a vaginal moisturizer
in baboons with decreasing ovarian
function, Lab Anim Sci 47:36-39, 1997.
42. Nachtigall LE: Comparative study: Replens versus
local estrogen in menopausal women,
Fertil Steril 61:178-180, 1994.
43. Bygdeman M, Swahn ML: Replens versus dienoestrol
cream in the symptomatic
treatment of vaginal atrophy in postmenopausal women, Maturitas
23:259-263, 1996.
44. Loprinzi CL et al: Phase III randomized double-blind
study to evaluate the efficacy of a
polycarbophil-based vaginal moisturizer in women with
breast cancer, J Clin Oncol
15:969-973,
1997.