CHAPTER 12
Orgasmic Difficulties In Women
Although not as prominent a sexual problem as
it once was, failure to achieve orgasm continues to be
a major complaint of many women. . . . the
manner, method, and ease of orgasmic attainment has
received wide publicity, and the woman who
does not regularly achieve orgasm feels deficient, deprived,
and often depressed.
Lieblum and Rosen, 19891
Prologue
Why are orgasm troubles in women considered
separately from phenomena
that are known by the same name in men? Is
there a difference
between the two? When considering only the
subjective sensation of
an orgasm, probably not. Masters &
Johnson,2
Kaplan,3 and DSM-IV4
do not separate men and women. Perhaps even
more tellingly, in a
study of written descriptions of orgasms
obtained from 24 men and 24
women, pronouns were deleted and the accounts
given to 70 health
professionals who were “blinded” men and
women.5
The
latter were
unable to distinguish the descriptions on the
basis of gender.
What about the equivalency of orgasm and the
word “sex?” For
many, the answer is that they are not the
same. A patient may be better
served if a clinician goes beyond a
consideration of orgasms only and
thinks also about sexual satisfaction.6 Clinical
experience suggests that
the meaning of orgasm to men and women is not
always the same.
Men tend to focus attention on their own and
their partner’s orgasms.
Many women also put great weight on the
intimacy and closeness that
accompanies a sexual experience.
The Problem
A 27-year-old single woman was concerned
about never having an orgasm. Since
her late teens, sexual experiences were a
regular and satisfying part of three longterm
and several brief relationships with men.
Despite her usual high level of
sexual desire and arousal and the absence
of discomfort with intercourse, as well
as her obvious pleasure with sexual
activity, partners often wondered why she was
not experiencing orgasm. They questioned if
they were somehow not “doing
something right” and generally gave the
impression that she was missing out on
a universal and gratifying sexual
experience. She wondered if something was
wrong with her sexual response. She felt
that her partners must be knowledgeable
about such issues, since they had the
wherewithal to compare her to other women
with whom they had had sexual experiences
(one was actually explicit in saying
so). Over the years, she read books and
articles in women’s magazines suggesting
masturbation as a way of learning to become
orgasmic but many attempts at selfstimulation
proved unsuccessful. Psychotherapy was
directed at focusing on her
sexual pleasure rather than whether or not
she experienced an orgasm. She was
still not orgasmic one year later but the
level of arousal that she experienced with
sexual activity had markedly increased. She
described herself as much more sexually
content.
Clinical experience suggests that the
meaning of orgasm to men and women
is not always the same. Men tend to
focus attention on their own and their
partner’s orgasm. Many women also
put great weight on the intimacy and
closeness that accompanies a sexual
experience.
In a study of written descriptions of
orgasms obtained from 24 men and 24
women, pronouns were deleted and the
accounts given to 70 health professionals
who were “blinded” men and
women.5 The
latter were unable to distinguish
the descriptions on the basis of
gender.
|
Terminology
“Climax” is often used as a synonym for
orgasm. On a colloquial level, the word “come”
has become the verbal equivalent of orgasm
(for women and men), and some women
use the more euphemistic words “peak” or
“satisfaction.”
Definition
Orgasm in a man is not difficult to detect,
since it is usually accompanied by ejaculation.
The process is more subjective in women,
although Masters and Johnson2 (pp.
128-137) described psychophysiological and
measurable phenomena associated with
female orgasm such as vaginal contractions.
They also described (p.5) three patterns in
the sexual response cycle experienced by
women. While two patterns reached the
level of orgasm, one (designated pattern “B”
[see Figure 3-2 in Chapter 3]), reached
sustained plateau level response without
orgasm apparently occurring. Since their first
book, Human Sexual Response, described
“normal” sexual anatomy and physiology, the
implication was thus left that the three
patterns of female sexual response were all
“normal” and so, too, was a high level of
female sexual response without orgasm.
Unfortunately, there was no commentary
accompanying the description of pattern “B”
so the frequency (as well as associated
changes in physiology, thoughts, and feelings)
of these women remains a mystery.
Classification
Female Orgasmic Disorder is defined in
DSM-IV-PC7
(p.
117) in the same terminology
as for the male: “Persistent or recurrent
delay in, or absence of, orgasm following a
normal sexual excitement phase. This can be
present in all situations, or only in specific
settings, and causes marked distress or
interpersonal difficulty. This diagnosis is
not appropriate if the difficulty in reaching
orgasm is due to sexual stimulation that is
not adequate in focus, intensity, and
duration.” Additional clinical information is provided:
“In diagnosing Orgasmic Disorder, the
clinician should also take into account
the person’s age and sexual experience. Once
a female learns how to reach orgasm, it
is uncommon for her to lose that capacity,
unless poor sexual communication, relationship
conflict, a traumatic experience (e.g.,
rape), a Mood Disorder, or a general medical
condition intervenes. . . .”
Two common clinical presentations of orgasmic
dysfunction in women are: (1) lifelong
and generalized (also called primary,
pre-orgasmia, anorgasmia, and lifelong
global) and (2) lifelong and situational
(also called situational and secondary). (The
term secondary can also refer to women
who not only experience orgasm through masturbation
but who do not experience orgasm “through any
type of partner stimulation
[and] who define their limited repertoire of
stimulation techniques leading to orgasm
as problematic”).8 A third
form of orgasmic dysfunction is that which is acquired and
generalized.
Clinicians commonly hear a concern from a
woman that she is experiencing orgasm
with masturbation (perhaps easily, and either
alone or with partner touch) but not during
penile-vaginal intercourse. Masters and
Johnson viewed the absence of orgasm
specifically during penile-vaginal
intercourse (while present otherwise), to be a disorder
requiring treatment9 (pp.
240-241). Many women objected to this idea, since it
seemed to echo a previously held idea that
orgasms experienced apart from intercourse
were considered “immature” in contrast to the
“mature” orgasms with intercourse. The
accumulation of epidemiological information
about patterns of orgasmic response in
women suggests that orgasm during intercourse
is not universal. In fact, one survey
found that the majority of respondents
in partner-related sexual activity usually came to
orgasm outside of penile-vaginal intercourse.10 This new
information resulted in a
change in the view of health professionals
treating women with orgasm concerns to
one of thinking that this pattern may not
represent pathology but “may constitute a
normal variation of female sexuality” 3 (p. 398).
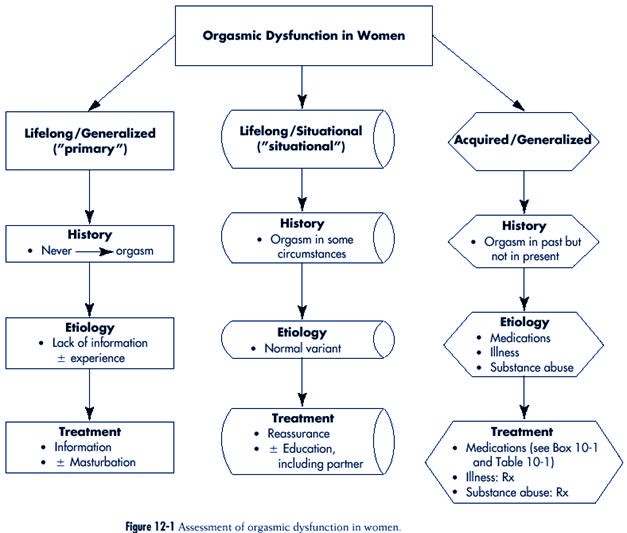
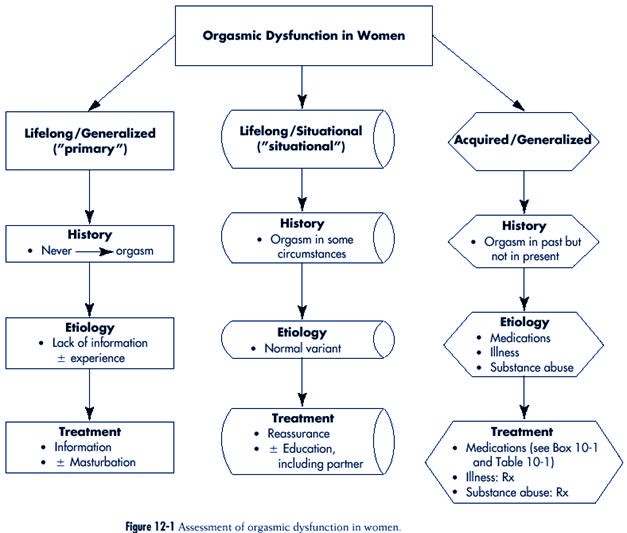
The assessment of orgasmic dysfunction in women
is outlined in Figure 12-1.
Description
Lifelong and Generalized (“primary”)
In the past, many women who reported a
lifelong and generalized history of orgasmic
dysfunction were considered to be otherwise
physically and psychologically
healthy. A woman with lifelong and
generalized orgasm would describe the following
symptoms:
1. Unlike other women she knew, she never had
an orgasm
2. She enjoyed sexual experiences with a
partner for the closeness but never felt
much sexual enjoyment
3. She never tried masturbation
4. She read little or nothing about sex and
orgasm
5. She talked to virtually no one about these
subjects
Today, women who are concerned about the
absence of orgasm often report:
1. A high level of sexual response when with
a partner and feeling close to “something”
2. Having read about sexual matters and
orgasm
3. Talking to partners about orgasm
4. Having “tried” to masturbate but finding
that it “didn’t work” (and possibly also
used a “toy” such as a vibrator)
Reports of masturbation attempts in the past
require more detailed questioning, since
they vary from meager (a few opportunities
for brief periods) to considerable (many
times involving great effort and lengthy
duration).
A recently married 26-year-old woman talked
to her family doctor about her sexual
response. Specifically, she said that while
she generally enjoyed sexual experiences
with men, she never had an orgasm by any
means whatsoever. She read in books
and women’s magazines about masturbation as
a way of experiencing orgasm, little
reservation about this approach, and tried
it but found it to be sexually frustrating.
When asked how many times she tried and for
how long, she related that she tried
about six times during a two-month period
about two years before, and for about
five minutes on each occasion. She stopped
trying when she experienced little
change in her sexual feelings. She also
reported that when male sexual partners
stimulated her clitoris, she generally
found this irritating and eventually asked them
to stop.
The patient’s doctor used the opportunity
of her periodic pelvic examination
and pap smear to explain aspects of female
genital anatomy and physiology, about
which the patient was not well informed.
This was done during the examination
by placing the patient in a semi-reclining
position while she held a mirror that
reflected her genitalia, so that she could
more easily understand the doctor’s
explanation.
After the examination, the patient was
encouraged to buy and read a self-help
book about women and orgasm and to
masturbate at home several times each
week for a much longer period of time (at
least 15 to 30 minutes) before she
stopped. When she returned as scheduled
three weeks later, the patient reported
the following:
• That she purchased and read the
recommended book
• That she experimented with
self-stimulation as suggested
• That she experienced a high level of
arousal in the process
She was encouraged to continue, and to
direct her husband in stimulating her
as she might do when alone. Three weeks
after that visit, she reported having
orgasms regularly when alone since shortly
after the previous visit. She also
described being less shy with her husband,
more candid in her directions, and
reaching a much higher level of arousal
with him. She was confident that orgasm
during sexual activity with her husband
would eventually occur.
Lifelong and Situational (“situational”)
Women who are situationally nonorgasmic on a
lifelong basis usually report that with
masturbation they have no difficulty coming
to orgasm. (Some may, alternatively,
describe infrequent orgasms with a partner.)
Some may be orgasmic with partnerrelated
sexual practices other than intercourse and,
in general, describe sexual experiences
as quite pleasurable. A lack of orgasm
usually extends over a lifetime of sexual
encounters for the woman (although it is not
unusual to hear that orgasm during intercourse
occurred once or a few times in the past).
Sometimes this pattern of response is
presented as a sexual concern. With greater
depth of questioning, the woman often
says that orgasms with intercourse would be
her preference if they could easily happen.
However, she states that she feels quite
satisfied if she can come to orgasm in
some form or another when with her partner,
(e.g., with oral stimulation) and that the
notion that this must occur specifically with
intercourse derives more from the wishes
of her partner rather than herself.
Acquired and Generalized
In the acquired and generalized form, the
woman reports the recent loss of the ability
to come to orgasm by any means whatsoever
with a partner or when alone, or alternatively,
a recent change in her sexual response
pattern such that orgasm occurs only
after an unusually lengthy process.
A 39-year-old woman was seen because she
recently became nonorgasmic. She was
in a harmonious lesbian relationship for
the past 10 years. The quantity of sexual
activity was considerably greater initially
but diminished over the years, largely
because of a discrepancy in sexual desire
between the two (the patient’s partner was
less interested). Sexual events were
qualitatively uncomplicated. In the past, both
were easily orgasmic and the patient
masturbated to orgasm several times each
week (an experience that she highly valued)
between sexual times with her partner.
She (the patient) had mild episodes of
depression in the past that were treated with
psychotherapy. However, more recently, she
had a more severe episode and she
accepted the inclusion of antidepressant
medication (an SSRI) in her treatment.
Within a week, she noticed that coming to
orgasm with masturbation was becoming
more difficult, and shortly after she found
that achieving orgasm became
impossible by any means (despite continued
desire and a high level of arousal).
Even though she felt improvement in her
mood, the medication was changed
because of the sexual side effect. When she
became orgasmic once again, however,
her symptoms of depression worsened. It
proved difficult to find a medication that
was effective in treating her mood problems
without also causing a loss of orgasm.
The benefit of the antidepressant was so
substantial that she chose abandoning her
orgasms for what she expected to be a
limited period of time.
Epidemiology
In response to a question in the Laumann et
al. study (“In the last 12
months, has there ever been a period of
several months or more when
you were unable to come to a climax?”) 24% of
women respondents said
“yes”.11 This was
the second most common sexual dysfunction reported
by women (the first was “lacked interest in
sex”). Orgasm difficulties in
women were more often associated (p. 371)
with the following:
1. Less education (30% of those who had “less
than HS”)
2. Low income (27% of those who were “poor”)
3. Impaired health (33% of those who were in
“fair” health)
4. Personal unhappiness (40% of those who
were “unhappy most
times”)
5. Younger age (less than 40 years old)
6. Marital status (highest [29%] in divorced
women)
7. Race (highest [29%] in black women)
8. Religion (highest [29%] in women who
reported “none”)
Information on subclassification can be
gained from a review of community based
research on the epidemiology of orgasmic
dysfunction in women.12 Various studies
show that 5% to 20% of women have never, or
infrequently, experienced orgasm. In
the language of DSM-IV-PC, such women would
be classified as having the lifelong
In response to a question in the Laumann
et al, study (“In the last 12
months, has there ever been a period of
several months or more when you were
unable to come to a climax?”) 24% of
women respondents said “yes”.11
This
was the second most common sexual
dysfunction reported by women.
|
and generalized form of orgasmic dysfunction.7 There is
inadequate data on the frequency
of the situational, and acquired and
generalized forms.
In a review of the frequency of orgasmic
problems in women as the presenting
problem in sex therapy clinics, there was a
reported range in several studies from 18 to
76%13 (p. 42). Variations
probably relate to the year the particular study was conducted
(several are from the 1970s and early 1980s)
and the focus of the clinic from
which the particular report emerged.
Etiology
Most of the comments about the etiology of
orgasmic dysfunction in women are
general and have not been made in relation to
any particular subtype. After reviewing
the literature on physiological,
sociological, psychological and interpersonal, and cultural
factors that might influence orgasm in women,
Morokoff concluded that
“. . . one association is clearly
uncontested: Birth later in the century is related to
higher frequency of orgasm14 (p. 156).
Whatever cultural changes in attitude toward
female sexuality are at work, it seems
possible that women who are better educated,
have higher social standing, and/or do not
have rigid religious morals have been
more easily influenced.”
Gebhardt related the experience of orgasm to
the extent of happiness of a woman
in her relationship. He found that a certain
group of women (35% to 41%) reached
“coital orgasm” regardless of the degree of
contentment.15
Since
the percentage was
appreciably higher (59%) in women from “very
happy” marriages, he concluded that
there were also women who were quite
sensitive to the state of their relationship and
who would not experience orgasm unless the
quality of this alliance was at a high
level.
While the importance of psychological issues
in the possible causes of orgasmic
dysfunction remain unclear from a research
perspective, they are difficult to ignore
clinically.
A 27-year-old woman, recently separated
after a five year marriage, was referred
because of never having been orgasmic. In
her previous sexual encounters, she was
usually interested, had no difficulty
becoming vaginally wet, and did not experience
pain with attempts at intercourse. She
described many of the physiological
phenomena associated with a high level of
arousal and felt herself “close,” at which
point “something would happen.” Her arousal
level and her feeling of sexual desire
would drop precipitously. The same pattern
existed with other partners before her
marriage, as well as with masturbation.
She wondered about sexual abuse during her
childhood but had no memory of
any such experience. However, she also
described a family-of-origin where her
father was uncommunicative, unaffectionate,
and critical. As an adult, she found
relationships with men difficult,
particularly in the areas of trust and control. She
felt that her distrusting attitude toward
men derived directly from her family and,
moreover, was underlined by her discovery
of a relationship between her husband
and another woman.
After one year of psychotherapy, she had a
better understanding of the origins
of her attitudes toward men and how they
shaped her life in the present. She also
felt more sexually responsive for longer
periods than had been the case in the past,
although to her chagrin, she remained
nonorgasmic. However, she was optimistic
that this situation might change.
Orgasmic dysfunction that is acquired and
generalized can result from various medications,
illnesses, and abused substances. However, as
compared to
impaired ejaculation/orgasm in men, there
seems to be considerably
less specific information in the literature
on the effects of these phenomena
on orgasm in women (see “Delayed
Ejaculation/Orgasm” in
Chapter 10). Segraves comments that women may
be less likely to
report orgasmic difficulty than men, since
they often are more prepared
to attribute the problem to an interpersonal
conflict than a biological
explanation.16 Although
his statement was made in relation to
antidepressant medications, it is equally
valid in other situations as well, and hence it
is necessary to ask specific questions when
determining the presence of side effects.
Some medications used in psychiatry, to
control high blood pressure and other ailments
seen in medical practice have a particular
predilection for interfering with the
orgasm part of the sex response cycle (see
Appendix III).17
Psychiatric
drugs that have
a specific effect on orgasm in women have
been reviewed.16,18,19
Antidepressants
(tricyclics,
MAOIs, and SSRIs), antipsychotics (some
phenothiazines), and antianxiety
drugs (some benzodiazepines) are reported as
causing anorgasmia in women. In a
recent (1997), comprehensive, and
family-practice-oriented report on the sexual side
effects of medications, Finger and his
colleagues provided information on all such
effects (not only those related to one part
of the sex response cycle), specified the
nature of the problems encountered, commented
on their relative frequency, and
included gender-specific observations (see
Appendix III).20
Some
of their notations are
relevant to the issue of orgasmic dysfunction
in women.
Some medical disorders result in symptoms
that affect orgasmic response for men
and women. Specific observations on diabetes21 and
multiple sclerosis (MS) in women22
are reported. One study on sexual problems in
women with MS refers to “difficulties”
in achieving orgasm. The authors of another
study23
on
the same subject found that
when a patient had genital sensory
disturbance, the kind of sexual practice that
occurred became significant when considering
whether or not the patient came to
orgasm. Three sexual practices were
described:
• Intercourse, least effective
• Oral stimulation, intermediate
• Manual stimulation, most effective
Studies of the effects on alcohol use on
sexual expression in women are confusing.
In a study of the effects of acute
intoxication on a group of 18 university women subjects,
24 alcohol was shown to result in a
progressively greater depressant effect on
Women may be less likely to report
orgasmic difficulty than men, since they
often are more prepared to attribute the
problem to an interpersonal conflict
than a biological one.16
|
orgasmic response as blood levels increased.
Specifically, alcohol was associated with
longer latency to orgasm and diminished
intensity of the feeling but, paradoxically,
greater sexual arousal and pleasure
associated with orgasm.
In an attempt to obtain more information on
the effects of alcohol on the sexual
activity of nonalcoholic women, a prospective
study involving daily logs of alcohol
intake and sexual activity was conducted on
69 subjects.25
Three
groups were
defined:
• No alcohol
• Moderate intake
• Heavy consumption
The only significant finding was that
female-initiated sexual activity occurred twice as
often without alcohol (versus with
alcohol). No significant effects were found on sexual
arousal, pleasure, or orgasm. These findings
indicate errors in retrospective accounts
on the stimulative effects of alcohol use on
sexual expression in women.
Investigation
History
History-taking provides core information.
Issues to inquire about and questions to ask
include:
1. Duration (see Chapter 4, “lifelong versus
acquired”)
Suggested Question: “How long has this
(not coming to orgasm)
been a concern to you?”
(Comment: asking about a non-experience is
admittedly rather awkward).
2. Partner-related sexual experiences other
than intercourse (see Chapter 4, “generalized
versus situational”)
Suggested Question: “Does your husband
(partner) touch your
genital area with his fingers or his mouth
during love making
(or sexual) times together?”
Additional Question: “Have you ever come
to orgasm that way?”
3. Masturbation experience (see Chapter 4,
“generalized versus situational”)
Suggested Question: “Have you had
experience with stimulating
yourself or masturbating?”
Additional Question if the Answer is Yes: “Have
you ever come to orgasm
with self-stimulation or masturbation?”
Additional Question: “Have you ever used a
vibrator?”
Additional Question if the Answer is Yes: “Did
you come to orgasm when
you did?”
4. Level of arousal (see Chapter 4,
“description”)
Suggested Question to a Woman who has not
Experienced an Orgasm: “If your
compare your sexual excitement to climbing a
mountain
and orgasm is the peak, what height do you
achieve when
the two of you make love?”
Additional Question if Husband (or partner) Touches
Woman with Hands or Mouth:
“What about when your husband (Partner)
touches you
with his hands or mouth?”
Additional Question if the Patient has
Experience with Masturbation or Use of a Vibrator:
“WHAT ABOUT WHEN YOU WERE MASTURBATING (OR
USING A
VIBRATOR )?”
Additional Question if Woman has been
Orgasmic: “Could you describe
what an orgasm feels like physically?”
“Psychologically?”
5. Psychological accompaniment (see Chapter
4, “patient and partner’s reaction to
problem”)
Suggested Question: “What are you thinking
about when you hope
for an orgasm and it doesn’t occur?”
Additional Suggested Question: “What does
your husband (partner)
say at such times?”
Physical Examination
The physical examination is usually
unproductive diagnostically in an apparently
healthy woman but can be important when
conducted for educational purposes.
Laboratory Examinations
No specific laboratory examinations appear
useful in an apparently healthy woman.
Treatment
Lifelong and Generalized
“Directed Masturbation” is the preferred
treatment method and, in principle, involves
education, self-exploration and body
awareness, and encouraging the patient to masturbate
to first experience an orgasm by herself
before expecting it to happen when
sexually active with a partner.26 The
objective of this approach is for the woman to
initially become comfortable with the
experience of orgasm when alone, with the hope
that she will subsequently feel equally
comfortable when experiencing an orgasm during
partner-related sexual activities such as
intercourse or oral stimulation. Alternatively,
or in addition, she could teach her partner
to stimulate her in the same manner
as she learned to stimulate herself. Several
studies have show this approach to be beneficial
and even superior to other treatment
procedures.27,28
Orgasm initially experienced through
masturbation was helpful to a great many
middle-class women in the 1970s and 1980s who
were born in North America and
continues to be widely used as a treatment
procedure. However, since the “sexual
revolution” in the 1970s, the availability of
books on the sexuality of women, sexual
information in women’s magazines, and the
appearance and discussion of explicit sexual
issues in movies, videos, and the Internet
have provided women (and men) with a
substantial amount of sexual information. The
resulting change in self-acceptance and
self-awareness has greatly affected all
aspects of the sexuality of women including
knowledge about body function generally and
orgasm specifically. As a consequence,
most adult women are better informed about
their body function in a sexual sense than
their counterparts in the 1970s and early
1980s. However, patients who have sexual
concerns sometimes avoid reading the
information available and may need encouragement
to do so. Primary care clinicians are in a
particularly advantageous position to
provide such assistance. Provision of
information and encouragement might be especially
valuable to certain groups of women such as
teens and adults who immigrated to
North America from countries where gender
roles are rigid and women are clearly
subservient to men (especially in relation to
sexual practices).
When supplying information and promoting the
directed masturbation
approach, one method is to proceed
step-by-step through the process
of learning to masturbate to the point of
orgasm. If the major
etiological factors are, indeed, lack of
sexual knowledge and experience,
the number of visits required and the extent
of health professional
involvement may be minimal and therefore
easily within the
pattern of practice in primary care. A less
time-consuming approach is
to suggest to the patient that she read and
use one of the readily available
self-help soft-cover books describing women’s
sexual response in
general10 and
masturbation techniques in particular.29,30 In a study that
has particular applicability to primary care,
a 15-session treatment program
was compared to a four-visit program.31 Both were
found to be
equally effective in helping the woman come
to orgasm with masturbation,
and the authors concluded that “ . . .
therapist contact time can be reduced
without loss of effectiveness” and that
lifelong and generalized orgasmic dysfunction
can be viewed as a “skill deficit.” One of
the self-help books29 also has an accompanying
videotape that many women find useful
(available through Focus International,
1-800-843-0305).
Many women are currently knowledgeable about
some sexual aspects of female
body function. However, many are unaware of
and curious about the details of female
genital anatomy (understandably, because the
vulva is ordinarily hidden from view and
comparisons between girls are therefore not
made in earlier developmental years, as
often happens with boys in school shower
rooms). Many women thus welcome the
In a study that has particular
applicability
to primary care, a 15-session treatment
program was compared to a fourvisit
program.31 Both
were equally
effective in helping the woman come to
orgasm with masturbation, and the
authors concluded that . . . “therapist
contact time can be reduced without loss
of effectiveness” and that lifelong and
generalized orgasmic dysfunction can be
viewed as a “skill deficit.”
|
reassuring opportunity to compare themselves
anatomically to others through the use
of a self-help book with color photographs
showing the panorama of vulvar shapes.32
Vibrators, fantasy, and Kegel’s exercises
have been suggested as adjuncts to directed
masturbation, particularly when ordinary
techniques do not achieve the objective of
the woman coming to orgasm. On the basis of
clinical experience, use of a vibrator can
be helpful, since the intensity of the
stimulation can not be matched by other methods.
Some professionals are concerned about the
development of dependency on a
vibrator3 (pp.
388-389); others are not28. Vibrators are easily available at
pharmacies,
department stores, and “sex” shops. No single
type is judged superior. Information
about vibrators is available in a specific
self-help book on this subject.33 Physicians can
arrange for vibrators to be “dispensed” by a
specific pharmacy to minimize patient
embarrassment.
Books and films that encourage the use of
erotic fantasy during sexual activity may
also be useful as an adjunct. In a study of
“reasonably normal married women,” the
occurrence of sexual fantasy during
intercourse was found to be common and one
conclusion derived was that it “could be used
adaptively to enhance sexual interest”.34
In another study, women with a sexual desire
disorder were found to have significantly
fewer sexual fantasies than controls who
described a “satisfactory sexual adjustment”.35
From these and other investigations, it is
thought that women with desire disorders
and other sexual dysfunctions might derive
benefit from creating fantasies if they did
not experience such phenomena in the ordinary
course of sexual events. Books describing
sexual fantasies in women can be used as a
method of assisting women in learning
to fantasize. An example of such a book is Herotica
2.36
In relation to the sexually arousing effects
of films on women, one study showed
that the subjective experience of arousal
appeared to be greater in women-made films
as compared to those made by men, although
the genital response to both was
described as substantial.37
Some clinicians also promote the use of
“Kegel’s exercises”.38 Kegel was a urologist
who taught women who were experiencing stress
incontinence to strengthen their
pubococcygeus muscle by repeatedly
contracting their perivaginal muscles. In the process
of doing this, some women reported an
increase in their perception of genital
sensations and in the frequency of orgasm.
Hence the notion was developed that such
exercises be used adjunctively in the
treatment of orgasmic dysfunction. In nondysfunctional
women (and consistent with Kegel’s original
observations), Kegel’s exercises
have shown to increase subjective ratings and
physiological measures of arousal.39
However, in women with orgasmic dysfunction,
such exercises have not proven to be
helpful with the lifelong and generalized
form or the situational form
(the latter despite an increase in
pubococcygeal strength).40 Whatever
beneficial effects exist may derive from an
increased focus of attention
of the patient on her genitalia.
LoPiccolo and Stock report that of
approximately 150 women
treated with directed masturbation, “about
95%” were able to reach
orgasm through masturbation.8 “Around
85%” were also able to come
to orgasm with the direct stimulation of a
sexual partner. “About 40%”
of these women were able to also experience
orgasms via penile-vaginal
intercourse.
In accordance with the concept that
orgasm with a partner (e.g., with touch
not including intercourse) is a normal
variation in the sex response cycle
experienced
by women, most clinicians who
treat people with sexual difficulties
approach this concern by “normalizing,”
and providing information and reassurance
to the patient.
|
Lifelong and Situational
In accordance with the concept that orgasm
with a partner (e.g., with touch but not
with the thrusting movements of intercourse)
is a normal variation in the sex response
cycle experienced by women, most clinicians
who treat people with sexual difficulties
approach this concern by “normalizing,” and
providing information and reassurance to
the patient. One aspect of this reassurance
is to help the patient place the issue of how
an orgasm occurs in perspective. Doing so
might involve clarification of the notion
that, while pleasure is one of the desired
“outcomes” of sexual activity and pleasure and
orgasm are connected, if the woman is left
feeling inadequate because orgasm does not
occur with a specific sexual practice, this
feeling could substantially interfere with her
sexual pleasure.
A 35-year-old married woman was referred
because she was anorgasmic. She was
seen alone because she was taking a summer
course in a city that was not where
she ordinarily lived. Her family remained
at home. In the course of history-taking,
it quickly became apparent that she
regularly and easily experienced orgasm with
touch (her own or her husband’s) but not
during intercourse, a situation that she
and her husband thought to be abnormal.
Information was given to her about the
variability of orgasm experiences in
different women, and reading matter on this
subject was suggested. When she returned
several weeks later for a second (and
final) visit, she summarized the interval
as follows:
1. She talked with her husband on the
telephone on the evening after the first
visit
2. She indicated that her own concerns had
greatly diminished
3. She reassured her husband about her
normality
4. The couple concluded that they did not
have any sexual difficulties
Verbal reassurance about the normality of not
experiencing orgasm during intercourse
is powerfully assisted by also referring the
patient to published information on this
subject. For example, the Hite Report
concerning sexuality in women declared that
about two thirds of the 3,000 women who were
surveyed reported that although they
were usually orgasmic, they did not have an
orgasm when penile-vaginal intercourse
was occurring.10
One method used to treat the concern about
not experiencing orgasm during intercourse
is to provide information about “the bridge
maneuver”41
(p.
87-93). This
approach initially involves the patient (with
fingers or vibrator) or her partner bringing
her to orgasm by direct clitoral stimulation,
and the partner then entering her vagina
while orgasm is taking place. Subsequently,
vaginal entry occurs just before orgasm
which, theoretically, would be provoked by
penile stimulation alone.
A 37-year-old woman, married for 12 years,
described a concern that she never had
orgasms during intercourse. Her husband
accompanied her to the appointment but
remained in the background. In response to
questions, he indicated that he was
supportive of what she wanted but at the
same time was quite content with their
present sexual experiences.
She was regularly and easily orgasmic alone
with masturbation and, as well,
when her husband stimulated her clitoris
with his fingers or orally. She was not
reassured when given information indicating
that her sexual and orgasmic response
pattern was within the range of normal.
However, she did not want to give up her
objective of orgasm during intercourse.
The approach used was to provide
information about the “bridge maneuver” to
the patient and her husband, and to see
them again in several weeks. During the
follow-up visit, both partners reported the
following:
1. Having tried the technique twice without
any change
2. Less concern on her part about how she
would experience orgasm
3. Both felt better about their relationship,
since they talked more about nonsexual
issues
Male partners tend to be more involved than
was the case in this story. In addition to
their current partner, women with orgasmic
difficulties have often been questioned in
the past about the sexual response of other
partners. Male partners often imply that
‘having an orgasm during intercourse is
important to my sexual pleasure and so it must
be for you too. If you are not having the
same kind of experience as I am, you must
not be enjoying yourself. Something is wrong
with this situation’. In addition, there is
an unvoiced (although sometimes voiced)
concern by the man that he is doing “something
wrong” and is therefore a “lousy lover.” The
man in this situation often seems to
have difficulty accepting his partner’s
reassurance. However, the same reassurance
given to the man from a health professional
authority seems to be quite powerful. Thus
it is important to see both partners
together.
Acquired and Generalized
Clarifying the possible etiological role of
medications, illness, or substance abuse is
essential if this is not already apparent to
the patient. Medications that interfere with
orgasm are outlined in Appendix III.
Strategies for managing delayed ejaculation/
orgasm resulting from medication use were
reviewed in Chapter 10 (see “Delayed
Ejaculation/Orgasm, Box 10-1, and Table
10-1). These same treatment approaches
apply to men and women.
Indications For Referral For Consultation Or
Continuing Care By A Specialist
1. Lifelong and Generalized: for the woman
who experiences this syndrome but
who is also sexually uneducated and
inexperienced a directed masturbation treatment
program with appropriate reading materials
should be implemented. For
the woman who is sexually educated and experienced,
the approach is not so
clear. If she is focused on orgasm rather
than her feelings of pleasure and does
not respond readily to reassurance about the
likely positive outcome, referral to
a sex specialist might be helpful.
2. Lifelong and Situational: most patients
respond positively to an approach that
normalizes their experience while at the same
time not minimizing their concern.
It may be essential to direct this message to
the partner as well. A patient
who does not want to accept this pattern as a
normal variant should be referred
to a sex therapist.
3. Acquired and Generalized: when orgasms
were a feature of a woman’s sexual
response in the past but cease to be so in
the present, a search for some biological
explanation should be made. A physician needs
to be involved if the
primary care professional is not an MD. When
a medication is found to interfere
with orgasm, the clinician should make use of
the information in Box 10-1
and Table 10-1 in Chapter 10. Illnesses and
substance abuse should be specifically
treated, since the sexual phenomena are
usually symptoms rather than disorders.
Clinicians must always consider the
possibility that disrupted sexual
function could be the presenting symptom of a
disorder rather than, for example,
the side effect of a medication.
Summary
Orgasmic dysfunction is the second most
common problem among women in the
general population (24%) but appears as less
of a clinical complaint then it did a
decade or two ago. When a concern does
surface, it can take one of three forms:
1. Lifelong and generalized (primary): the
woman never had an orgasm by any
means (5% to 10% of women)
2. Lifelong and situational: the woman is
orgasmic by one means (e.g., masturbation)
but not by other means (e.g., intercourse)
(very common)
3. Acquired and generalized: the woman has
lost the capacity that she once had to
come to orgasm (infrequent in a healthy
population).
History-taking is essential in the
investigation of the complaint of orgasmic dysfunction
(physical and laboratory examinations are
distinctly less helpful [other than for
educational and reassurance purposes]) in an
apparently healthy woman. The lifelong
and generalized form is usually a result of
lack of awareness of sexual issues affecting
women and is responsive to educational input
and initial experience of orgasm through
masturbation. The concept of the generalized
and situational form as a problem requiring
treatment has changed substantially so that
today this pattern is considered a “normal”
variant of female orgasmic response. Women
with this concern are generally
responsive to reassurance although this often
involves the partner as well. The acquired
and generalized form usually results from
medication side effects, symptoms of illness,
or direct effects of abused substances. When
a side effect of medications is responsible
(see Appendix III), several treatment
approaches (see Box 10-1 and Table 10-1 in
Chapter 10) can be employed. Only in the
occasional instance does specialized care
seem necessary for any of the three forms
described.
REFERENCES
1. Leiblum SR, Rosen RC: Orgasmic disorders in women
(introduction). In Leiblum SR,
Rosen RC (editors): Principles and practice of sex
therapy: update for the 1990s, New York, 1989,
The Guilford Press, pp. 51-88.
2. Masters WH, Johnson VE: Human sexual response, Boston,
1966, Little, Brown and
Company.
3. Kaplan HS: The new sex therapy: active treatment of
sexual dysfunctions, New York, 1974,
Brunner/Mazel, Inc.
4. Diagnostic and statistical manual of mental
disorders, ed 4, Washington, 1994, American
Psychiatric Association.
5. Vance EB, Wagner NN: Written descriptions of orgasm: a
study of sex differences, Arch
Sex Behav 5:87-98, 1976.
6. Jayne C: A two-dimensional model of female sexual
response, J Sex Marital Ther 7:3-30,
1981.
7. Diagnostic and Statistical Manual of Mental
Disorders, ed 4, Primary Care Version, 1995,
Washington, American Psychiatric Association.
8. LoPiccolo J, Stock WE: Treatment of sexual
dysfunction, J Consult Clin Psychol
54:158-167, 1986.
9. Masters WH, Johnson VE: Human sexual inadequacy, Boston,
1970, Little, Brown and
Company.
10. Hite S: The Hite report: a nationwide study
on female sexuality, New York, 1976, Macmillan.
11. Laumann EO et al: The social organization of
sexuality: sexual practices in the United States,
Chicago, 1994, The University of Chicago Press, pp.
35-73.
12. Spector IP, Carey MP: Incidence and prevalence of the
sexual dysfunctions, Arch Sex
Behav 19:389-408, 1990.
13. Wincze JP, Carey MP: Sexual dysfunction: a guide
for assessment and treatment, New York, 1991,
The Guilford Press.
14. Morokoff PJ: Determinants of female orgasm. In
LoPiccolo J, LoPiccolo L (editors):
Handbook of sex therapy, New York,
1978, Plenum Press, pp. 147-165.
15. Gebhard PH: Factors in marital orgasm, Journal of
Social Issues 22:88-95, 1966.
16. Segraves RT: Overview of sexual dysfunction
complicating the treatment of depression,
J Clin Psychiatry Monograph 10:4-19,
1992.
17. Crenshaw TL, Goldberg JP: Sexual pharmacology:
drugs that affect sexual function, New York,
1996, W.W. Norton & Company.
18. Segraves RT: Psychiatric drugs and inhibited female
orgasm, J Sex Marital Ther
14:202-207, 1988.
19. Shen WW, Sata LS: Inhibited female orgasm resulting
from psychotropic drugs: a fiveyear,
updated clinical review, J Reprod Med 35:11-14,
1990.
20. Finger WW, Lund M, Slagle MA: Medications that may
contribute to sexual disorders: a
guide to assessment and treatment in family practice, J
Fam Prac 44:33-43, 1997.
21. Zemel P: Sexual dysfunction in the diabetic patient
with hypertension, Am J Cardiol
61:27H-33H, 1988.
22. Lundberg PO: Sexual dysfunction in female patients
with multiple sclerosis, Int Rehab Med
3:32-34, 1980.
23. Hulter BM, Lundberg PO: Sexual function in women with
advanced multiple sclerosis, J
Neurol Neurosurg Psychiatry 59:83-86,
1995.
24. Malatesta VJ et al: Acute alcohol intoxication and
female orgasmic response, J Sex Res
18:1-17, 1982.
25. Harvey SM, Beckman LJ: Alcohol consumption, female
sexual behavior, and
contraceptive use, J Stud Alc 47:327-332, 1986.
26. LoPiccolo J, Lobitz WC: The role of masturbation in
the treatment of orgasmic
dysfunction, Arch Sex Behav 2:163-171, 1972.
27. Kohlenberg RJ: Directed masturbation and the
treatment of primary orgasmic
dysfunction, Arch Sex Behav 3:349-356, 1974.
28. Riley AJ, Riley EJ: A controlled study to evaluate
directed masturbation in the
management of primary orgasmic failure in women, Br J
Psychiatry 133:404-409, 1978.
29. Heiman JR, LoPiccolo J: Becoming orgasmic: a
sexual and personal growth program for women,
editor revised and expanded, New York, 1976, Prentice
Hall Press.
30. Barbach LG : For yourself: the fulfillment of
female sexuality, New York, 1975, Anchor Books.
31. Morokoff PJ, LoPiccolo, J: A comparative evaluation
of minimal therapist contact and
15-session treatment for female orgasmic dysfunction, J
Consult Clin Psychol 54:294-300,
1986.
32. Blank, J: Femalia, San Francisco, 1993, Down
There Press.
33. Blank, J: Good Vibrations: the complete guide to
vibrators, San Francisco, 1989, Down There
Press.
34. Hariton BE, Singer JL: Women’s sexual fantasies
during sexual intercourse: normative and
theoretical implications, J Consult Clin Psychol 42:313-322,
1974.
35. Nutter DE, Condron MK: Sexual fantasy and activity
patterns of females with inhibited
sexual desire versus normal controls, J Sex Marital
Ther 9:276-282, 1983.
36. Bright S, Blank J: Herotica 2: a collection of
women’s erotic fiction, New York, 1991, Down There
Press.
37. Laan E et al: Women’s sexual and emotional responses
to male- and female-produced
erotica, Arch Sex Behav 23:153-169, 1994.
38. Kegel AH: Sexual functions of the pubococcygeus
muscle, West J Surg Obstet Gynecol
60:521-524, 1952.
39. Messe MR, Geer JH: Voluntary vaginal musculature
contractions as an enhancer of sexual
arousal, Arch Sex Behav 14:13-28, 1985.
40. Chambless DL et al: Effect of pubococcygeal exercise
on coital orgasm in women,
J Consult Clin Psychol 52:114-118,
1984.
41. Kaplan HS: The illustrated manual of sex therapy, ed
2, New York, 1987, Brunner/Mazel, Inc.