Despite the current rhetoric. . .
. about sex and intimacy’s involving more than penile-vaginal intercourse,
the quest for a rigid erection
appears to dominate both popular and professional interest. Moreover,
it seems likely that our
diligence in finding new ways for overcoming erectile difficulties serves
unwittingly to reinforce the male
myth that rock-hard, ever-available phalluses are a necessary component
of male identity. This is indeed
a dilemma.
Rosen and Leiblum,
19921
General Considerations
The Problem
A 49-year-old widower described erection
difficulties for the past year. His 25-year
marriage was loving and harmonious
throughout but sexual activity stopped after
his wife was diagnosed with ovarian cancer
six years before her death. Their sexual
relationship during the period of her
illness had been meager as a result of her lack
of sexual desire. Although he missed her
greatly, he felt lonely since her death
three years before and, somewhat
reluctantly at first, began dating other women. A
resumption of sexual activity soon resulted
but much to his chagrin he found that
in contrast to when he would awaken in the
morning or masturbate, his erections
with women partners were much less firm. He
felt considerable tension, particularly
because some months before, he had
developed a strong attachment to one
woman in particular and was fearful that
the relationship would soon end because
of his sexual troubles. As he discussed his
grief over the loss of his wife and talked
about his guilt over his intimacy with
another woman, his erectile problems began
to diminish.
A 67-year-old man, married for 39 years,
and having a history of angina prior to a
coronary by-pass operation three years
before was referred to a “sex clinic” together
with his wife because of his erectile
difficulties. Sexual experiences had been enjoyable
and uncomplicated for both until he
developed angina at the age of 62.
Orgasm provoked his chest pain.
Nitroglycerin was prescribed but he used it only
occasionally because it resulted in
headache. His angina during sexual activity was
frightening to his wife who, nevertheless,
recognized the importance of sexual
experiences in his life and supported his
desire to continue being sexually active.
Cardiac surgery resulted in the
disappearance of his chest pain. However, some
months before his operation, he began to
experience difficulty becoming fully
erect at any time, and would frequently
lose whatever fullness he had before vaginal
entry occurred. His erectile difficulties
with his wife had become persistent
and when questioned, it was apparent that
his morning erections were not different.
Sildenafil (Viagra) was dismissed as a
treatment possibility because of his occasional
use of nitroglycerin. He was referred to a
urologist for intracavernosal injections.
Terminology
The phrase “erectile dysfunction”
has provided competition for the more popular word
“impotence.” The latter has a
tenacity for usage that does not exist for the female
equivalent and now rarely-seen
word, “frigidity.” Both words have similar deficiencies:
they are so broad in usage they
(1) incorporate disorders of desire and function and
(2) imply something pejorative
about the patient’s personality quite apart from their
sexual expression.2
The social confusion surrounding
the word “impotence” is, perhaps, exemplified by
the first recommendation of the
National Institutes of Health Consensus Statement on
Impotence, which was to change
the term impotence to erectile dysfunction as a way of
characterizing “the inability to
attain and/or maintain penile erection sufficient for satisfactory
sexual performance.”3
(Interestingly, no conference was necessary to change
usage of the word “frigidity”).
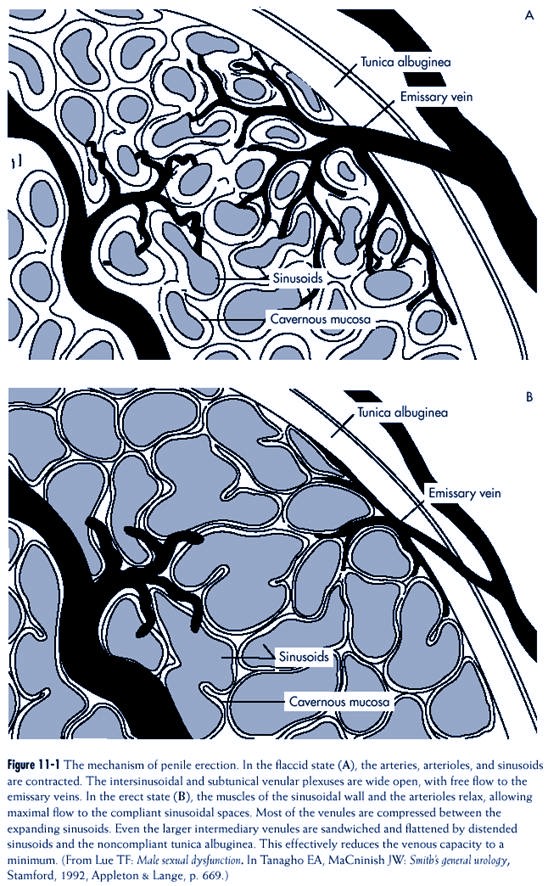
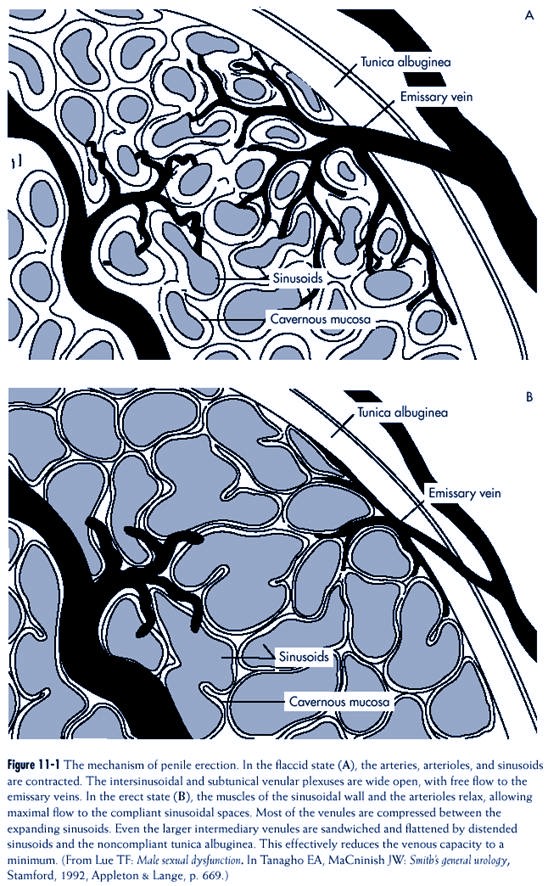
Mechanism of Erection
The fundamental element in the
development of an erection is the trapping of blood
in the penis. The mechanism by
which this occurs was described by Lue and Tanagho
(Figure 11-1). A human penis has
three cylinders: Paired corpora cavernosa (CC) on
the dorsal surface, and the completely
separate corpus spongiosum (CS), which carries
the urethra and is responsible
for the ventral bulge.
The CS anatomically includes the
glans of the penis. The CC are each surrounded
by an inflexible envelope of
fibrous tissue: the tunica albuginea (TA). The CS has a
much thinner TA and is connected
to the glans, which has almost none.
Blood is carried to the penis by
the two internal pudendal arteries
and within the penis by paired
cavernosal arteries. The latter subsequently
divide into smaller vessels
(arterioles), which are surrounded
by smooth muscle. The same can be
said of the helicine arteries (small
spiral shaped arteries). In the
CC and CS, blood is then carried to
interconnecting sinusoids
(microlakes, which have the appearance of a
sponge when filled but are mostly
collapsed when a penis is flaccid),
which are also surrounded by
smooth muscle. Small veins (venules)
carry blood away to the emissary
veins, which in turn pierce the TA.
As an erection develops, there is
relaxation of the smooth muscle
around the arterial tree and
walls of the sinusoids, increasing the inflow
As an erection develops, the smooth
muscle around the arterial tree and
walls of the sinusoids relaxes, increasing
the inflow of blood into the penis and
allowing more blood to remain. While
expansion occurs, the venules are
compressed
between the sinusoids and TA,
thereby stopping the outflow and in
effect trapping blood in the sinusoids of
the penis.
|
of blood into the penis and
allowing more blood to remain. While expansion occurs,
the venules are compressed
between the sinusoids and TA, thereby stopping the outflow
and in effect trapping blood in
the sinusoids of the penis. “The smooth muscles
in the arteriolar wall and
trabeculae surrounding the sinusoids are the controlling
mechanism of penile erection.”4
(Biochemical aspects of erection
are discussed in the treatment section of “ Generalized
Erectile Dysfunction: Organic,
Mixed, or Undetermined Origin” below in this
chapter).
Definition
The main difficulty with the
definition of erectile dysfunction is whether the diagnosis
of erectile problems should refer
only to the hardness or softness of a man’s erection
or if it should also include a
behavioral component. For example, should a man
who has erections that are
persistently partial but whose penis is sufficiently enlarged
to regularly engage in
intercourse be designated as having an “erectile disorder?” If
that same man designates himself
as “impotent,” what should be the diagnostic position
of the health professional?
Should there be a subjective component to an erectile
disorder: does it make any
difference what the man (or his partner) thinks? Is the
fullness of a man’s penis in
intercourse all that matters? Is intercourse the only sexual
activity on which the definition
is based? What about erections with other sexual
practices? These, and other
questions, are not intellectual exercises but daily clinical
quandaries.
Classification
DSM-IV-PC summarized the criteria
for the diagnosis of “Male Erectile
Disorder” as follows: “persistent
or recurrent inability to attain, or to
maintain until completion of the
sexual activity, an adequate erection,
causing marked distress or
interpersonal difficulty”5(p. 116).
The clinician
is further instructed to
“especially consider problems due to a general
medical condition . . . such as
diabetes or vascular disease, and
problems due to substance use . .
. such as alcohol and prescription
medication. Erectile
dysfunction in all situations, as well as lack of nocturnal erections,
strongly suggests
that a general medical condition
or substance use is the cause”(italics added).
The subclassification of Erectile
Disorders used in this chapter is summarized in
Figure 11-2.
Epidemiology
The Massachusetts Male Aging
Study (MMAS) provided revealing information about
erectile function, dysfunction,
and “potency” in middle-aged and older men.6 The
study was conducted in the late
80s, was concerned with health and aging in men, was
community-based, and involved a
random sample of noninstitutionalized men 40 to 70
years old. Individuals who
completed a self-administered questionnaire on sexual function
and activity included 1290 (75%)
of the 1709 MMAS subjects. “Potency” was
subjective in that it was defined
by those who completed the questionnaires. Defined
as “satisfactory functional
capacity for erection,” “potency” could “coexist with some
Erectile dysfunction in all situations,
including the lack of nocturnal erections,
strongly suggests that a general medical
condition or substance use is the cause.5
|
degree of erectile dysfunction in
the sense of submaximal rigidity or submaximal capability
to sustain the erection.” Four
degrees of “impotence” were described:
• None
• Minimal
• Moderate
• Complete
The overall prevalence of
impotence in this study was found to be
52%, with 15% defined as minimal,
25% moderate, and 10% complete.
Prevalence was highly related to
age with the probability of moderate
impotence doubling from 17% to
34% and complete impotence tripling
from 5% to 15% between subject
ages 40 to 70 years. Looking at
this from the opposite
perspective, 60% of men were not impotent at
age 40 years, compared to 33% not
impotent at age 70 years.
The frequency of erectile
problems found in health care settings seems to depend
somewhat on the clinical context.
That is, different percentages can be found in
various clinical settings:
medical outpatients, urology, and sex therapy7 (p.
11). In a
review of the frequency of sexual
problems presented to “sex clinics” between the
mid-70s to 1990, 36% to 53% of
men complained of “male erectile disorder.”8 Masters
and Johnson subcategorized this
diagnosis into “primary” and “secondary”.9 The
former referred to a man who had
never had intercourse (p. 137), and the latter
referred to a man who had been
able to have intercourse at least once in the past
Sixty percent of men were not impotent
at age 40 compared to 33% not impotent
at age 70 years.
|
(p.157). Of all the men with
“impotence” who consulted Masters & Johnson, 13%
had the primary form (p. 367).
Etiology
“Repeatedly bandied about is the
hackneyed declaration that in the 1970s, mental
health professionals pronounced
90% of impotence to be psychogenic; more recently
urologists proclaim that 90% of
impotence is organic. Both sides are wrong, not just
for the disrespectful attitudes
toward one another, but for failing to develop more
sophisticated notions of
etiology.”10
LoPiccolo saw clinical
limitations to the either/or approach and suggested an
alternative way of thinking about
the etiology of erectile dysfunctions: that organic
and psychogenic factors be viewed
as two “separate and independently varying
dimensions” and that both should
be examined in each instance.11 To
support this
position, he reported on 63 men
with erectile difficulties who were carefully and
thoroughly investigated in both
areas. Ten men were found to have a purely psychogenic
etiology, and three men were
found to have a purely organic etiology.
The majority of men in this study
(50/63) displayed a mixture of factors, indicating
that a “two-category typology was
. . . inappropriate.” Furthermore, almost
one third of the men (19/63) had
“mild organic impairments” but “significant psychological
problems.” These men might have
been considered “organic” in a twopart
etiological scheme, however, they
might also have been sufficiently responsive
to psychological intervention
such that physical treatment may not have been necessary.
In a diagnostic and a therapeutic
sense, the implication of LoPiccolo’s approach is
quite serious. It means that even
if a factor that is of potential etiological significance is
found (biological or
psychological), it is not necessarily the factor. Or, in other words,
“the detection of some possible
etiological factor . . . does not mean that the
cause . . . has been fully
explained. Such a factor may even be coincidental, of no
(actual) etiological
significance.”12
The possible nature of the
interrelationship between biological and psychological
factors was suggested as the
following: “When any one (organic factor) occurs in isolation,
it may serve to make erections
more vulnerable to emotional disturbances and
sympathetic overactivity,
facilitating the vicious circle of performance anxiety that
maintains ED.”12
Investigation
History
History-taking is an
indispensable element in the investigation of erectile disorders
and provides direction for
further exploration and treatment. Issues to inquire about
and questions to ask include:
1. Duration (see Chapter 4,
“lifelong versus acquired”)
Suggested Question: “Have you
always had difficulties with erections
or is this a relatively new
problem?”
2. Partner-related erections (see
Chapter 4, “generalized” versus “situational”)
Suggested Question: “What are
your erections like when you are
with your wife (partner)?”
3. Sleep [including morning]
erections (see Chapter 4, “generalized versus situational”)
Suggested Question: “What are
your erections like when you
wake up in the morning?”
Additional Question: “Do you
wake up at night for any reason?”
Additional Question if the Answer
is Yes: “What are your erections like
when you wake up at night?”
(Comment: the assessment value of
asking about sleep-related erections is generally
recognized but not universally
accepted.13 When full sleep-related erections exist, the
information seems highly useful
from a diagnostic viewpoint. However, partial or nonexistent
sleep erections are not
necessarily meaningful since this situation may coexist
with daytime erections firm
enough for intercourse.)
4. Masturbation erections (see
Chapter 4, “generalized versus situational”)
Suggested Question: “What are
your erections like when you stimulate
yourself (or masturbate)?”
5. Fullness of erections (see
Chapter 4, “description”)
Suggested Question: “On a
scale of zero to ten where zero is
entirely soft and ten is fully
hard and stiff, what are your
erections like when you are with
your wife (partner)?”
Additional Question: “Using
the same scale, What are your erections
like when you wake up in the
morning?”
Additional Question: “If you
wake up during the night, using the
same scale, what are your
erections like at that time?”
Additional Question: “using
the same scale, What are your erections
like with self-stimulation
or masturbation?”
Additional Question Under All
Three Circumstances: “About how long do
your erections LAST?”
(Comment: Even though erections
may be full under all three circumstances, the duration
of erections may be important.
Erections may consistently be short-lived—a matter
of diagnostic significance, since
that observation may indicate a “venous leak”).13
6. Psychological accompaniment
(see Chapter 4, “patient and partner’s reaction to
problem”)
Suggested Question: “When you
have trouble with your erection,
what’s going through your mind?”
Additional Question: “What
does your wife (partner) say
at these times?”
Physical Examination
In men with erectile
difficulties, physical examination is essential even
if the “yield is low.”12
“Without it many patients feel that they have not
been properly assessed or taken
seriously and they may refuse a psychogenic
diagnosis as a result”.12
The physical examination concentrates
particularly on the endocrine,
vascular and neurologic systems,
as well as local genital factors.
Signs of hormonal abnormalities
include the following14 (p. 85):
1. Testicular atrophy
2. Gynecomastia
3. Galactorrhea
4. Visual field abnormalities
5. Sparse body hair
6. Decreased beard growth
7. Skin hyperpigmentation
8. Signs of thyroid abnormalities
9. Low energy level and lack of
“well-being”
Signs of vascular disease include
the following14 (p.91):
1. Weak pulses in legs or ankles
2. Hair loss on lower legs
3. Unusually cool temperature of
penis or lower legs
4. High lipid levels
5. High cholesterol levels
6. Duputyren’s contractures
[Peyronie’s disease only]
7. Fibrosis of outer ear
cartilage [Peyronie’s disease only]
Signs that indicate neurological
factors include the following14 (p. 93):
1. Weak or absent genital
reflexes (bulbocavernosus, cremasteric, scrotal, internal
anal, and superficial anal)
In men with erectile difficulties, physical
examination is essential even if the
“yield is low.”12 Many
patients feel that
they have not been properly assessed or
taken seriously if there is no physical
examination, and they may refuse a
psychogenic diagnosis as a result.12
2. Neurological abnormalities in
the S2 to S4 nerve root distribution
3. Reduced penile sensory
thresholds to light touch electrical stimulation or
vibration
An investigation conducted in a medical
outpatient clinic found that the physical
examination rarely helped to
differentiate various etiological factors with two exceptions15:
• Small testes in patients with
primary hypogonadism
• Peripheral neuropathy in
patients with diabetes
Laboratory Investigation
The extent of a clinician’s use
of the laboratory in the investigation of erectile dysfunction
depends on the results of the
history and physical examination (see “Investigation”
below in this Chapter in the
sections on “Situational [‘psychogenic’] Erectile Dysfunction”
and “Generalized Erectile
Dysfunction: Organic, Mixed, or Undetermined Origin.”
Treatment
As LoPiccolo has shown,
psychological and physiological factors are
present in the vast majority of
men with an erectile disorder.11 “Psychological”
factors include social, cultural,
religious, and interpersonal
elements, and those within the
person. Since all sexual behavior of men
is influenced to a great degree
by these issues, it is reasonable to
assume that these factors are
present in the context of erectile difficulties
as well. The logical result of
LoPiccolo’s research is the concept
that regardless of the etiology
of a man’s erectile difficulties, a health care clinician
must always attend to universally
concomitant psychological issues. That is:
“Given the critical role of
psychological factors, even in cases with clearcut organic
etiology, the failure to
attend to psychological issues is indefensible (italics added). The
potential
impact of erectile difficulties
on mood state, self-esteem and self-efficacy, as well as on
the couple’s relationship cannot
be overemphasized.”16
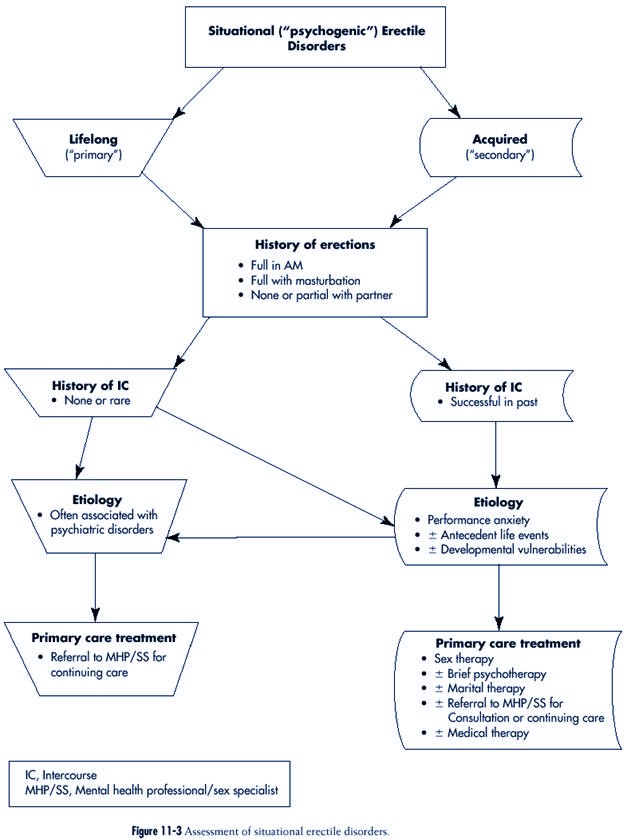
Situational (“Psychogenic”) Erectile Dysfunction
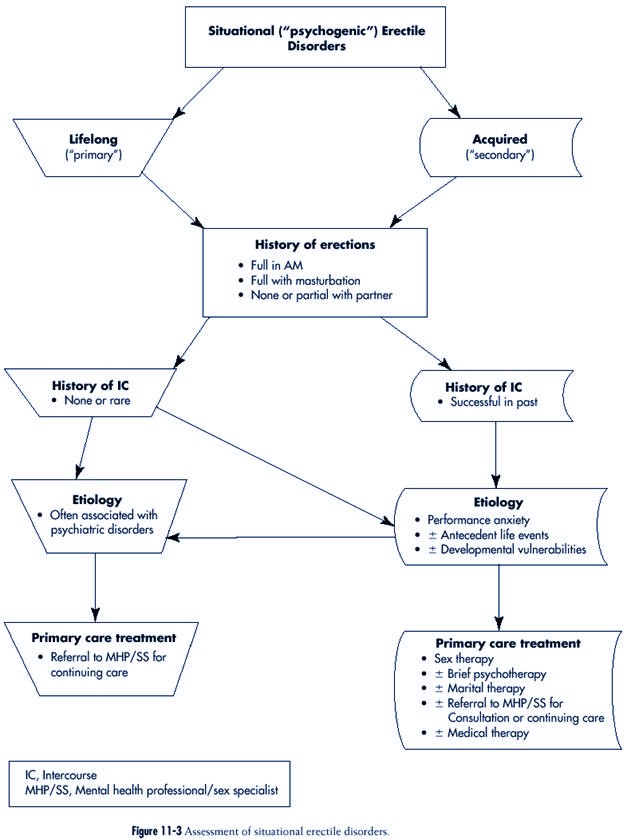
The assessment of situational
erectile disorders is summarized in Figure 11-3.
Description
Lifelong (“Primary”) Erectile Disorders
In this unusual syndrome, the man
reveals that all, or most, attempts at intercourse
result in diminution of his
erection before attempts at vaginal entry. Levine reasonably
suggested that the definition of
the disorder be “liberalized” to include men who
gain vaginal entry “occasionally”17
(p. 208), Typically, the man has no difficulty
obtaining full erections when
alone, with masturbation, or when awakening. Ejaculation
and orgasm have been similarly
unimpaired. The sexual desire phase may have
been problematic if thoughts
associated with sexual arousal were atypical (as is
Failure to attend to psychological issues
is indefensible. The potential effect of
erectile difficulties on mood state,
selfesteem,
and self-efficacy (as well as the
couple’s relationship) cannot be
overemphasized.16
often the case), such as
fantasies related to paraphilias. Since behavior connected to
such fantasies is often easier to
carry out alone, such men tend to avoid intimate
relationships and may depend on
prostitutes (with whom they can be more candid)
for partner-related sexual
experiences. Even then, intercourse rarely, if ever, occurs.
Pressure from a (non-prostitute)
partner may be a major factor in seeking treatment.
When this occurs, the patient may
not be particularly forthcoming about his thoughts
and feelings.
A 32-year-old man was seen with his
29-year-old wife. They were married for two
years and despite being sexually active
with one another several times each week,
intercourse never occurred. (They
previously agreed not to engage in intercourse
before they married.) She was aware of the
fact that he had never experienced
intercourse in the past. His erection
predictably diminished whenever he moved
close to her vagina. She wanted to become
pregnant and felt the “biological clock
ticking.”
Her desire for pregnancy and her love for
her husband resulted in a singleminded
pursuit of her attempts at solving their
sexual difficulties. He was less
enthusiastic. Attempts at psychotherapy
with him alone and sex therapy as a
couple proved unhelpful. Since he was a shy
person and spontaneously revealed
little about himself, he never previously
told anyone about having been repeatedly
sexually assaulted as a child by his mother.
Nor had he ever discussed his
current sexual fantasies (about which he
was quite ashamed) that involved the
insertion of a knife into a woman’s vagina.
He was again referred for individual
psychotherapy and accepted the need for
candor with his therapist concerning
his sexual experiences as a child and his
current sexual thoughts and feelings.
Acquired (“Secondary”) Erectile Disorders
In contrast to the lifelong form
of situational erectile dysfunction, the patient
reports having had intercourse in
the past, perhaps on many occasions for many
years. However in the present,
full erections might occur with his partner before
clothes are removed but the
fullness may diminish after he reaches the bed or
after the commencement of sexual
activity. Intercourse might occur sometimes but
this seems unpredictable.
Characteristically, he never had a problem obtaining full
erections after a period of sleep
and with masturbation and, as well, describes no
difficulty with ejaculation and
orgasm now or in the past. History reveals that
when younger, he frequently had
erection troubles with partners on the first few
occasions when sexual intercourse
was attempted. However, when in a long-term
relationship, he functioned well
sexually although erectile difficulties occasionally
reappeared at times of “stress.”
After a relationship of many years, doubts about
his sexual “performance”
developed. There may have been a marked diminution of
sexual activity in spite of his
partner’s attempts at reassurance. She believed him
not to be sexually interested,
and wondered about her own attractiveness to him.
Questioning revealed that his
apparent sexual disinterest is actually avoidance. He
remains privately interested but
feels that he is not “a man” anymore with his
wife.
A 51-year-old rather shy man was seen
together with his 49-year-old outspoken
wife. They were married for 23 years.
Sexual activity had never been a problem
until about five years ago when his
erections sometimes became soft after vaginal
entry, so much so that intercourse could
not continue. This sequence of events,
and erectile loss even before intromission,
gradually occurred more often and
culminated in the complete lack of
intercourse in the previous six months. His
sexual desire, while never as strong as
that of his wife, had not changed and he
would masturbate (without erectile problem)
and ejaculate about once or twice
each month. He thought that the origin of
his erection troubles were mainly
related to his age but he also wondered if
his substantial use of alcohol for the
previous 25 years was also a factor. His
heavy drinking stopped completely about
five years ago when he joined AA. This was
about the same time that his erection
problems began. After discussion of
possible etiological factors, he understood
that much of his erectile difficulty was
connected to his feelings about his wife.
They were referred to a treatment program
that focused on both their marriage
and their sexual relationship.
Etiology
Lifelong (“Primary”) Erectile Dysfunction
This syndrome is “often, though
not invariably, associated with a diagnosable major
[psychiatric] condition”18
(p. 133). Masters and Johnson described a group of 31
men with “Primary Impotence,”
eleven of whom were in unconsummated marriages9
(pp. 137-156). Factors they
considered to be of etiological significance were multiple
and included the following:
1. Homoerotic desire
2. Mother/son incest
3. Strict religious orthodoxy
4. Psychologically damaging
attempts at first intercourse with a prostitute (sometimes
associated with drugs or alcohol)
Other investigators also reported
associated paraphilias and gender
identity disorders18
(pp. 133-135);19 (p. 245).
Acquired (“Secondary”) Erectile Dysfunction
Most men with a clearly
situational erectile dysfunction also indicate
that it is acquired.
In almost all such men, the
etiology involves some combination of
factors17(p.
200) in the following three areas:
1. Performance anxiety
In almost all men with acquired erectile
dysfunction, the etiology involves a
combination of factors17
in three areas:
1. Performance anxiety
2. Antecedent life events
3. Developmental vulnerabilities
|
2. Antecedent life events
3. Developmental vulnerabilities
The “phase of time” for each of
these three is, respectively, here-andnow
lovemaking, months to years
(“recent” history), and childhood/
adolescence (“remote” history).
A major here-and-now issue is
“performance anxiety,” a concept
introduced by Masters and Johnson
to describe the worry that a patient
may have about his or her sexual
function and whether it will be similarly
impaired on a current occasion as
it was at a previous time.9 Performance
anxiety is partner related and
probably universal in men with
erectile difficulties. From a
primary care perspective, performance anxiety
is an important target of the
treatment of “psychogenic impotence”
in both solo men and couples.
However, this component explains only
part of the etiology of this
syndrome, since eliminating performance
anxiety does not always result in
cure.
Antecedent life events and
developmental vulnerabilities may be of
therapeutic significance also,
but they are difficult to consider in detail
in a primary care setting.
The former “typically fall into
one of five categories”17 (p.202):
1. Deterioration in the nonsexual
relationship with a spouse or
partner
2. Divorce
3. Death of a spouse
4. Vocational failure
5. Loss of health
Developmental vulnerabilities
include such issues as child sexual abuse and impairments
in sexual identity.17
On a clinical level, one
frequently has the impression of a link between psychogenic
erection difficulties and
difficulty with expression of anger. In the MMAS study,
the suppression and expression of
anger was assessed. “Men with maximum levels of
anger suppression and anger
expression showed an age-adjusted probability of 35%
for moderate impotence and 16% to
19% for complete impotence, both well above
the general level (9.6%).”6
The MMAS study did not subcategorize men with “impotence”
according to whether the origin was
“psychogenic,” “organic,” mixed,” or
“undetermined.” It may certainly
be possible that problems with anger may also
potentiate some of the
etiological factors associated with erectile difficulties of
organic, mixed or undetermined
origin discussed below.
Laboratory Investigation
If in instances where the man
reports being otherwise healthy, the history clearly
indicates the situational nature
of the man’s erectile dysfunction, there is no sign of
any contributory physical
abnormality, and there are no other sexual symptoms (such
as lack of sexual desire), little
needs to be done to obtain additional specific laboratory
data.
Performance anxiety is partner related
and probably universal in men with
erectile difficulties.
Developmental vulnerabilities include
child sexual abuse and impairments in
sexual identity.17
Antecedent life events typically fall into
one of five categories17:
1. Deterioration in the nonsexual
relationship
2. Divorce
3. Death of a spouse
4. Vocational failure
5. Loss of health
Eliminating performance anxiety does
not always result in cure.
|
Treatment
“It is fortunate for many
psychologically impotent men that a complete
understanding of the causes is
not necessary. Some men spontaneously
get over their problem within a
short period of time without
any therapy”17
(p. 202). For those whose problem is not solved,
an approach is proposed that
concentrates on five themes that have
been identified in a review of
the literature (Box 11-1).16 Most
importantly for generalist health
professionals, some of these five
themes listed in Box 11-1 can be
easily integrated into primary
care.
The first theme is accurate
information and realistic ideas and expectations regarding
sexual performance and
satisfaction—all of which is a problem in many
men with erectile difficulties
(and their women partners).
Areas to be addressed include:
1. Genital anatomy and physiology
2. The sex response cycle
3. Masturbation
4. Male-female differences in
sexual response
5. Effect of aging, illness, and
medication on sexual desire, arousal, and
orgasm
Comprehensive, inexpensive, and
up-to-date self-help books are easilly
vailable and can be used as an
adjunct in this education process.20 The
provision of information can
correct unrealistic ideas and expectations—
thoughts that could, themselves,
significantly interfere with erectile function.
For example, the “gold standard”
of erectile function for many men is what occurred in
their teenage years. The folly of
“living in the past” becomes evident to a man in his
(for example) 40s when he is
asked to provide another example of a part of his body
that functions in the present as
it did when he was a teenager. In addition, it could be
pointed out to him that he is, in
effect, basing his sexual expectations for his 60 years
of adult sexual function
(approximate life expectancy minus 15 years of pre- and early
Box 11-1
Themes in the Treatment of Situational (“Psychogenic”) Erectile
Dysfunction
• INFORMATION, including realistic ideas
and expectations concerning sexual performance
and satisfaction
• PERFORMANCE ANXIETY RELIEF through use of
“sensate focus”
• ”SCRIPT” MODIFICATION (‘who does what to
whom’)
• ATTENTION TO RELATIONSHIP ISSUES (e.g.,
intimacy, control, conflict resolution,
trust)
• RELAPSE PREVENTION
|
Areas to be addressed include:
1. Genital anatomy and physiology
2. The sex response cycle
3. Masturbation
4. Male-female differences in sexual
response
5. Effects of aging, illness, and
medication
on sexual desire, arousal, and
orgasm
Easily-available, comprehensible and
comprehensive, inexpensive, and up-todate
self-help books can be used as an
adjunct in this educational process.20
The “gold standard” of erectile function
for many men is what occurred in their
teenage years. The folly of “living in the
past” becomes evident to a man in his
(for example) 40s when he is asked to
provide another example of a part of
his body that functions in the present as
it did when he was a teenager.
|
adolescence) on the five (or so)
years of erectile experience as a teen! Other examples
of ideas and expectations that
might be discussed with a patient include his thoughts
when he or his partner is
initiating sexual activity and when his penis is becoming
firmer or softer.
Yet another example of the
therapeutic value of information is that of the sexual
changes associated with aging.
The educational effect on the treatment of erectile
dysfunction was studied in a
group of heterosexual couples between the ages of 55 and
75.21 Investigators
found that a four-hour workshop resulted in increased knowledge,
especially about the normal
changes that occur with age, thereby allowing participants
to have more realistic
expectations of themselves and their partners. Sexual satisfaction
also increased despite the
presence of associated organic factors.
The second theme is the relief of
“performance anxiety.” Diminishing or eliminating this
frequently appearing factor
involves inducing sexual response in the man (in this
instance, erection) while he
paradoxically avoids sexual invitations for intercourse.
Masters and Johnson described
this approach to the treatment of performance anxiety9
(pp. 193-213). The method
involves couple oriented touching “exercises” and
concentrates on sensate focus,
a term they coined (pp. 71-75) to denote a focus on
immediate sensation rather than
sexual goals of, for example, intercourse. Briefly, the
exercises occur in stages and
initially exclude intercourse and touching of breasts (in
the woman) and genitalia, then
include touching of the previously barred areas (while
maintaining the exclusion of
intercourse), and finally include unrestricted touching
and intercourse. Couples do not
move to the next level of the exercise until the previous
one is mastered. While requiring
repeated visits, this technique
is not complex and might,
therefore, be within the boundaries of primary
care (depending on the
clinician’s time, comfort, and interest
and the availability of
specialists to whom one could refer).
One major (and often unappreciated)
objective of “sensate focus” in
the treatment of erectile
dysfunction is change in the communication
pattern between partners so they
could, with “permission” (i.e., encouragement),
and with a minimum of tension and
embarrassment, tell one
another what is, and is not,
pleasurable. (Rather than the communication exercise it is,
sensate focus is sometimes
mistakenly thought of as a way of allowing one to discover
previously unappreciated physical
feelings in particular body areas.) A second objective
of “sensate focus” is to remove
the demand for intercourse. Since the man does not
“need” an erection for any
purpose other than intercourse and intercourse is not to take
place, theoretically the
“pressure” on the man to “perform” will be removed and the
worry (which is thought to
inhibit his erection) will disappear, thus allowing his erection
to develop unhindered.
Two obstacles to sensate focus
have been described11 (p. 189). First, the
passive
process of sensate focus is
contrary to the need of aging men for
active and direct penile
stimulation for an erection to develop. Second,
the idea of performance anxiety
is so popular that general knowledge
of the concept has rendered its
treatment less effective. Consequently,
LoPiccolo coined the term metaperformance
anxiety to explain
Rather than the communication exercise
it is, sensate focus is sometimes
mistakenly
thought of as a way of allowing
one to discover previously unappreciated
physical feelings in particular body
areas.
Functional men can become aroused on
demand, whereas the same request in
dysfunctional men results in interference
with the arousal process.
|
why, on some occasions,
“eliminating performance anxiety does not lead to erection
during sensate focus body
massage”11 (p. 189).
Recently the role of “anxiety” in
producing erectile troubles and the expected relief
with its disappearance has been
reexamined and reviewed from a research rather than
clinical viewpoint.22
Functional and dysfunctional men have been shown to respond
differently to anxiety. The
results of these studies are summarized as follows:
1. Functional men can become
aroused on demand, whereas the same request in
dysfunctional men results in
interference with the arousal process (similar results
were found in laboratory studies)
2. Functional men report their
subjective arousal to be greater than dysfunctional
men regardless of what occurs
physically
3. (Particularly interesting from
a therapeutic viewpoint) functional
men report distraction to be an
obstacle to sexual response, whereas
this is neutral or actually
helpful to dysfunctional men16
The third theme concentrates on
sexual “script” modification (i.e., changes to
what actually occurs sexually
between two people). The fourth theme concentrates on relationship
issues such
as intimacy, control, conflict resolution, and trust. The fifth theme
concentrates
on the prevention of relapse.
Since the third, fourth, and fifth areas are often more
within the interests, practice
pattern, and skills of the sex therapist, they are not discussed
at length here.
Little published information
exists on the treatment of situational erectile dysfunction
by methods usually reserved for
occasions when the etiology is “organic, mixed,
or undetermined” (see below in
the chapter). Few quarrel with the concept of considering
such an approach when
psychologically-oriented methods have been unsuccessful.
However, when medical techniques
are used early in the course of treatment, the concept
is more problematic. The
rationale sometimes given is one of providing the man
an opportunity to have a erection
in worry free circumstances as a way of overcoming
an undefined obstacle. The
rationale continues that after the man
engages in successful sexual
experiences that require an erection he will
be able to do so without extra
support.
A study of the use of
intracavernosal injections in 15 men with “psychogenic
impotence” did not convey a sense
of optimism about the
outcome of such an approach.23
The authors concluded that performance
anxiety was not alleviated, that
dependence on injections for
intercourse remained, and that
the capacity for intimacy did not
improve. One can well imagine
that the consequences (benefits and
disappointments) of the use of
such treatments for men with situational
erectile difficulties become
magnified when men who have these problems
ask for, and are given, an oral
medication such as sildenafil (see below in the
chapter).
Few long-term follow-up studies
have been conducted on the treatment of erectile
dysfunction. Results for
“primary” and “secondary” (i.e., acquired) erectile dysfunction
were reported by Masters and
Johnson as an “overall failure rate” (OFR)
and were based on personal
interviews conducted five years after the patients were
Functional men report distraction to be
an obstacle to sexual response, whereas
this is neutral or actually helpful to
dysfunctional
men.16
A study of the use of intracavernosal
injections in 15 men with “psychogenic
impotence” did not convey a sense of
optimism about the outcome of such an
approach.23 The
authors concluded that
performance anxiety was not alleviated,
that dependence on injections for
intercourse
remained, and that the capacity
for intimacy did not improve.
|
originally treated9
(p. 367). The OFR for “primary impotence” was 41%. This modest
improvement supports the clinical
experience of greater complexity in the treatment
of this form of the erectile
dysfunction syndrome. Furthermore, it suggests
that insofar as “primary”
impotence is concerned, a focus on performance anxiety
without considering other factors
will likely result in quite limited gains.
The OFR reported by Masters and
Johnson for the “secondary” form was 31%.9
Another follow-up study in the
United States, carefully conducted after three years,
found that of the 18 men
presenting with “difficulty achieving or maintaining erection,”
ten maintained the improvement,
four were the same, and three were worse.24
The authors found that there was
“significant improvement maintained across time in
erectile capability during
intercourse . . . . improved satisfaction in the sexual relationship
. . . [and] . . . longer duration
of foreplay.” Hawton and his colleagues
conducted a rigorous one to six
year follow-up study in the United Kingdom and
found that the “gains made during
therapy by couples who presented with erectile
dysfunction were reasonably well
sustained.”25 Of the 18 couples who undertook treatment,
14 reported the problem resolved
or mostly so at the end of therapy, and 11
reported the same at follow-up.
Indications for Referral for Consultation or Continuing
Care by a Specialist
1. Since the “primary” form of
situational erectile disorders is so often associated
with complex individual
diagnosable psychiatric conditions rather than interpersonal
conflicts, referral to a mental
health professional for individual treatment is
usually the most reasonable
course of action19 (p. 245). If the health
professional
is not also a sex-specialist, it
may be useful to consult with one before proceeding
with the referral.
2. Solo men with the “secondary”
form of situational erectile dysfunction (i.e.,
those without a partner, with an
uncommitted partner, in a relationship that is
filled with so much discord that
they are unable to cooperate with each other, or
who have been raised in a culture
in which men are clearly in control and women
entirely submissive) often
require an amalgam of traditional psychotherapy and
sex therapy. Such men are
candidates for individual care with a sex-specialist
who is also a mental health
professional.
3. Couples in which the man has
the “secondary” form of situational erectile dysfunction
and who would benefit by a
here-and-now focus on information and
performance anxiety (previously
described in the treatment of situational problems
in this chapter) could be cared
for in primary care. Couples who do not
respond to this approach may
require an additional focus on two of the other
elements: “script” modification
and attention to relationship conflicts. Given the
time and experience involved in
providing these other components, referral
would be reasonable in these
circumstances. If referral does take place, the health
professional should be a
sex-specialist who also has clinical experience in the
mental health area.
4. Consultation with a
sex-specialist is warrented when consideration is given to
providing a form of treatment
usually reserved for men with erectile dysfunction
of “organic, mixed, or
undetermined origin.” The purpose would be to examine
the possibility of integrating
biological and psychologically oriented treatment
methods.
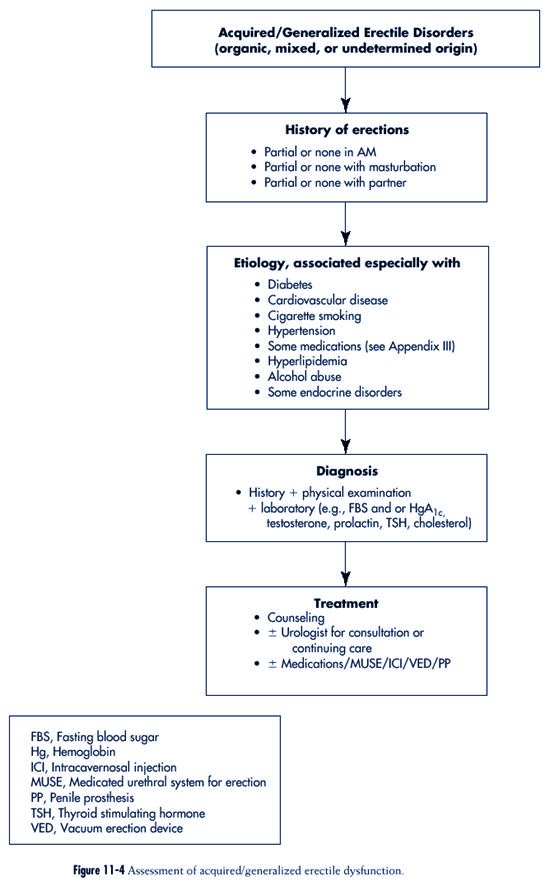
Generalized Erectile
Dysfunction: Organic, Mixed,
or UnDetermined Origin
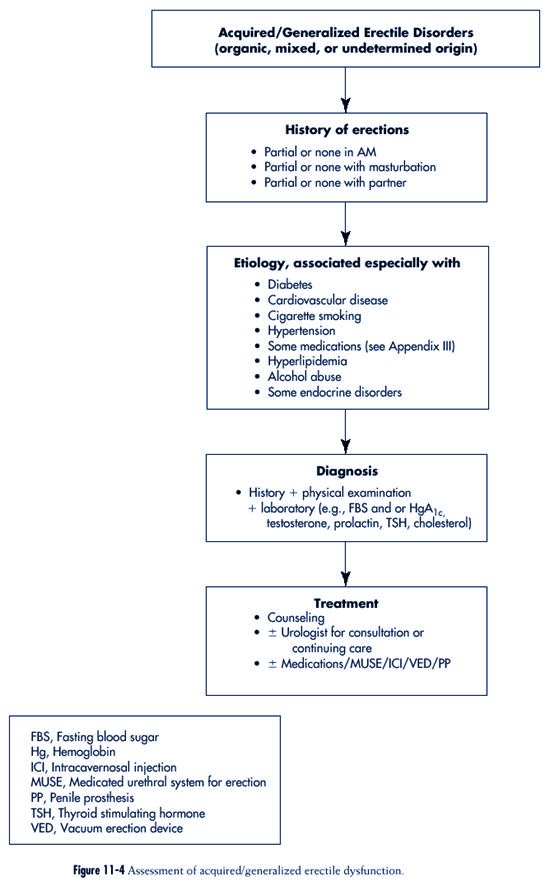
The assessment of generalized
erectile disorders is summarized in Figure
11-4.
Description
The key differentiating feature
of the acquired and generalized form of
erectile dysfunction is that the
difficulty experienced by the man exists
in all major circumstances when
he would be expected to have an erection:
with a partner, masturbation, and
with sleep (including the time
when he awakens in the morning).
In addition, he describes little or no
difficulty with erectile function
in the past. Typically in his 50s or
older, his erection problems
began in recent years. Sexual desire is usually
present but, depending on the
status of his health and the nature of any previous
health troubles, there may have
been problems with ejaculation or orgasm. Relationship
conflict was not apparent except
as a possible result of reluctance to seek help
despite his partner’s
encouragement. Although unhappy, he is not clinically
depressed.
A couple in their mid-60s were seen because
of the man’s erectile difficulties. They
were married for seven years, both for the
second time. Five years before, he held
an executive position in a major computer
software company but as a result of
“downsizing” lost his job and subsequently
retired. His wife had always been in
good health but he had a “mild” heart
attack about three years before. He felt well
since then, stopped smoking, and was not
taking any medications. On his last
medical visit several months earlier, he
talked with his physician about erection
troubles, which had begun about one year
before. Further history-taking revealed
that the fullness of his erections during
sexual activity with his wife (as well as in
the morning and with masturbation—which
occurred once every few months) had
become consistently about 50% of what he
had previously experienced. The last
time he could recall having a full erection
at any time was about one year earlier.
He was referred to a urologist and after a
thorough investigation he was told that
the reason for his trouble was “organic.”
Intracavernosal injections were suggested.
He was reluctant to pursue this option and
wanted a second opinion from a sex
therapist. This consultation primarily
confirmed the opinion of the urologist and as
a result he began injection treatment. He
changed to sildenafil (Viagra) when this
became available and after three months of
use, he and his wife reported that they
were pleased with the results.
The key differentiating feature of the
acquired and generalized form of erectile
dysfunction is that the difficulty
experienced by the man exists in all
major circumstances when he would be
expected to have an erection: with a
partner, masturbation, and with sleep
(including the time when he awakens in
the morning).
|
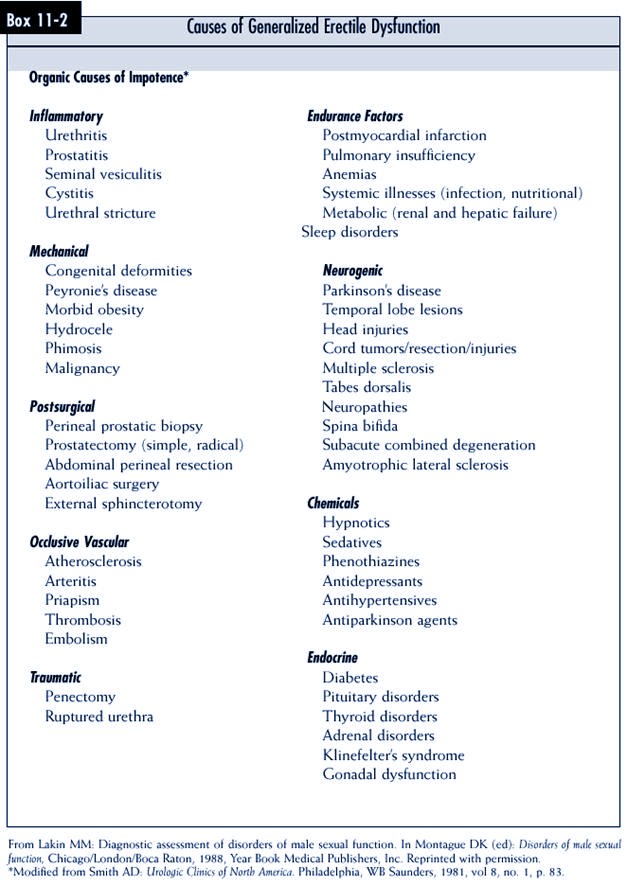
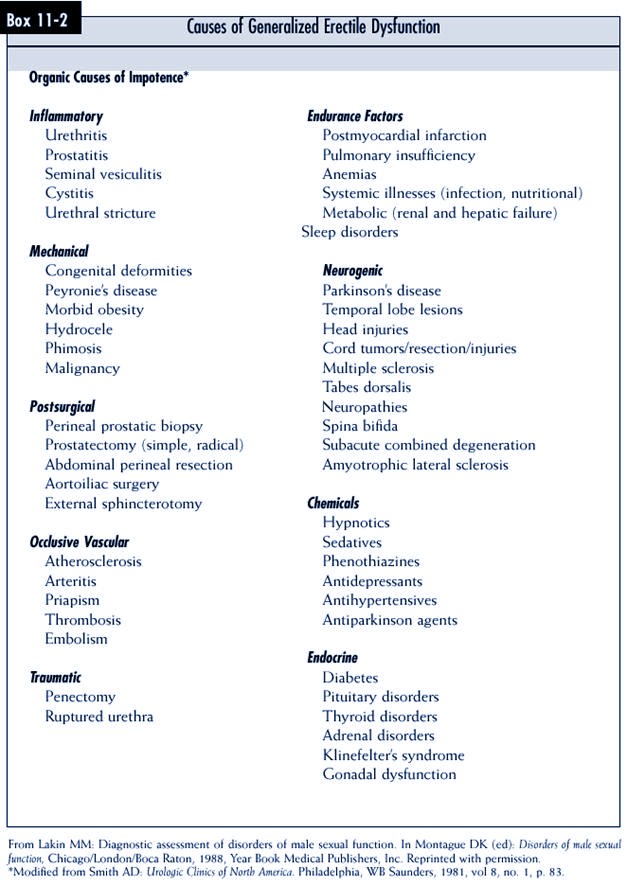
Etiology/Risk Factors
Many medical disorders are
identified as “organic causes” of erection difficulties (see
Box 11-2), however, only a few
seem to account for a great many cases where the
etiology is known. Major
etiological factors are discussed below.
In the Massachusetts Male Aging
Study, health status was ascertained by asking if
diabetes, heart disease, and
hypertension were present.6 These
three “were significantly
associated with changes in the
impotence probability pattern.” After
adjusting for age, 28% of men
with treated diabetes, 39% of men with
treated heart disease, and 15% of
those with treated hypertension were
described as having “complete
impotence.”
Diabetes
Estimates of the prevalence of
erection problems in men with diabetes
range from 27% to 71%.26
As many as 50% of people with type 2
diabetes remain undiagnosed
(about 8 million people in the United
States), a serious situation since
hyperglycemia in this condition
causes microvascular disease and
may contribute or cause macrovascular
disease.27 Erection
problems may well be a manifestation of microand/
or macrovascular disease. In the
MMAS sample, “the age-adjusted
probability of complete impotence
was three times greater in subjects
reporting treated diabetes than
in those without diabetes.”6 In an
attempt to clarify
the connection between diabetes
and erection problems and to eliminate the confounding
effects of associated illness and
medications, 40 men with diabetes (but free
of other illness or drugs apart
from antidiabetic medication) were compared to an
equivalent group of age-matched
healthy controls.26 The men with diabetes were
found to have a wide variety of
sex-related difficulties, including:
1. Erectile dsyfunction with
attempts at intercourse, during sleep, and with masturbation
2. Sexual desire disorders
3. Diminished frequency of
intercourse
4. Premature ejaculation
5. Diminished sexual satisfaction
In another study, sexually
functional men with diabetes were shown to have significantly
diminished Nocturnal Penile
Tumescence (NPT) profiles when compared to a similar
control group.28
Cardiovascular Disorders
The association between erectile
difficulties and cardiovascular disorders is well studied.
“Vascular disorders” include two
groups: arterial (i.e., obstruction to the penile
inflow tract) and veno-occlusive
(i.e., the inability to trap blood in the corpus cavernosum).
29 The former has attracted
particular attention.
The presence of four arterial risk
factors (ARF) (diabetes, smoking, hyperlipidemia,
and hypertension) was assessed in
440 “impotent” men.30 The frequency of “organic
Forty men with diabetes with no other
illnesses and taking no drugs other than
antidiabetic medication were compared
to the equivalent group of age-matched
healthy controls.26 The
men with diabetes
were found to have a variety of sexrelated
difficulties, including erectile
function with attempts at intercourse,
during sleep, and with masturbation;
sexual desire; frequency of intercourse;
premature ejaculation; and sexual
satisfaction.
|
impotence” occurred in 49% of men
without any ARF, and 100% when there were
three or four risk factors.
Cigarette Smoking
The link between cigarette
smoking and arterial disease is well established.
Smoking was found to be
significantly more prevalent in men
who were “impotent” compared to
estimates of smoking among men in
the general population.31
In one study, two groups of men with and
without penile arterial disease
were compared, and the former was found
to have smoked more pack-years.32
In the MMAS, “complete impotence”
was higher in current smokers
(versus current nonsmokers) who were also treated
for heart disease, hypertension,
or arthritis, and, as well, in those taking cardiac drugs,
antihypertensives, or
vasodilators.6 In subjects with treated heart disease the
probability
of “complete impotence” in the
MMAS was 56% for current smokers compared to 21%
for current nonsmokers. Likewise,
treated hypertension together with smoking increased
the probability of “complete
impotence” to 20% of those who had both
factors, as compared to 9% among
hypertensive men who did not
smoke. Apart from particular
connections between smoking and other
risk factors, “a general effect
of current cigarette smoking was not
noted.”
Hypertension
The relationship between
“impotence” and “erection dysfunction” and
hypertension was examined in a
review of studies that were conducted in the 1970s
and 1980s33(p.
204). Impotence was found in 7% of men with normal blood pressure.
Impotence was found in 17% to 23%
of untreated men with hypertension and in 25%
to 41% of men who were treated
for hypertension. From these studies, the association
between “impotence” and hypertension
(apart from drugs used in its treatment) is
clearly evident.
Lip ids
In the MMAS, a negative
correlation was found between “impotence” and high density
lipoprotein cholesterol, although
this was not so with total serum cholesterol.
“In the older men (age 56 to 70
years), the age-adjusted probability
of ‘moderate impotence’ increased
from 6.7% to 25% as high
density lipoprotein cholesterol
decreased from 90 to 30 mg./dl.”6
Medications
A variety of drugs used presently
and in the recent past have been shown
to interfere with erectile
function in men (see Appendix III). The increase
in the number of new drugs that
are currently being introduced for various
human ailments and the increased
speed with which they appear on
the market make it likely that
unanticipated side effects (including sexual
side effects) of these agents
will become apparent only after they
have been used for a period of
time. Physicians must therefore be constantly
sensitive to the possibility of
sexual side effects (including effects
Impotence was found in 7% of men with
normal blood pressure. Impotence was
found in 17% to 23% of untreated men
with hypertension and in 25% to 41% of
men treated for hypertension.33
The increase in the number of new
drugs that are currently being introduced
for various human ailments and
the increased speed with which they
appear on the market make it likely
that unanticipated side effects (including
sexual side effects) of these agents will
become apparent only after they have
been used for a period of time. Physicians
must therefore be constantly sensitive
to the possibility of sexual side
effects (including effects on the mechanism
of erection) of newer drugs.
In the MMAS, “complete impotence” was
higher in current smokers (versus current
nonsmokers) who were also treated
for heart disease, hypertension, or
arthritis, and, as well, in those taking
cardiac drugs, antihypertensives, or
vasodilators.6
|
on the mechanism of erection) of
newer drugs. The following comment was made about
hypotensive agents but applies
equally to other drugs as well: “Although . . . certain
agents . . . . are likely to have
sexual side effects [while] other agents . . . are unlikely
to be associated with erectile
dysfunction, it is important to stress that any agent may
cause erectile difficulties in
certain patients . . . there is [also] considerable individual
variation in vulnerability of
erectile function to different drugs. In other words, the existing
literature can only serve as a
general guide to patient management”
(italics added)34 (pp. 111-112).
In the MMAS study, “complete
impotence” was found to be present significantly more
often in men taking the following
medications than in the sample as a whole (10%)6:
• Hypoglycemic agents (26%)
• Antihypertensives (14%)
• Vasodilators (36%)
• Cardiac drugs (28%)
This association was not found
with lipid-lowering drugs.
Two groups of drugs
(antihypertensives and medications used in psychiatry)
have been particularly implicated
in the development of erectile
dysfunction33
(pp. 197-337).
Issues learned from sexual side
effect research on antihypertensive
drugs (that apply to other
substances as well) include the following
items32 (pp.
206-207):
• Possibility of late appearance
(6 months or more)
• Lack of information about their
effects on women
• Importance of assessing sexual
symptoms of the underlying
disease
• Need to include information
from partners
• Usefulness of information about
masturbation
• Need to assess alcohol use and
abuse
Alcohol
“With just a few drinks, most men
experience transient boosts in sex drive and sociability.
With continued drinking, however,
erection and ejaculation abilities systematically
decrease in a dose-related
fashion to a point of total dysfunction.”
32 Although there are acute
and chronic effects of alcohol on sexual
function, comments here focus on
the latter. Studies relating to chronic
alcoholism and epidemiology,
Nocturnal Penile Tumescence (NPT),
hormonal and neurologic effects
have been reviewed.35
An examination of clinical
experience in the care of approximately
17,000 male alcoholics over 36
years revealed that 8% spontaneously
described continued erectile
problems after detoxification.36 Years
later,
despite abstinence, 50% had not
fully recovered their erectile function.
The continuation of sexual desire
in these men indicates that their erectile problems
were unlikely to be simply a
result of insufficient testosterone but rather more fundamental
structural and functional body
changes, including:
• Effect on testosterone
receptors
Issues learned from sexual side effect
research on antihypertensive drugs
include the possibility of their late
appearance (6 months or more), the
lack of information about their effects
on women, the importance of assessing
sexual symptoms of the underlying disease,
the need to include information
from partners, the usefulness of
information
about masturbation, and the
need to assess alcohol use and abuse32
(pp. 206-207).
An examination of clinical experience in
the care of approximately 17,000 male
alcoholics over 36 years revealed that
8% spontaneously described continued
erectile problems after detoxification.36
Years later, and despite abstinence, 50%
had not fully recovered their erectile
function.
|
• Influence of estrogen
• Damage to organs in the body,
including the central nervous system,
testicles, and liver
• Existing diseases caused or
made worse by alcohol abuse such as diabetes,
heart disease, and peripheral
neuropathy
In addition, two controlled
studies on the effects of alcoholism on sexual function
demonstrate that erectile
dysfunction37 and also desire problems38
were more common
in alcoholic men.
In an effort to assess the effect
of alcohol use on NPT, 26 sober, healthy, sexually
functional, and medication-free
chronic alcoholics and controls were studied for two
nights in a laboratory setting.39
The subjects had fewer full penile tumescent episodes
that were also shorter in
duration. The authors speculated on the possible contribution
of central processes to the
effects of alcohol on erections.
The impact of chronic alcoholism
on pituitary-gonadal function appears at both
levels. Apart from liver disease,
chronic alcoholic men show evidence of hypogonadism,
abnormalities in spermatogenesis,
and testicular atrophy.40 Such men
also demonstrate
diminished androgens, elevated
estrogens, and increased prolactin levels.
The neuropsychiatric effects of
chronic alcoholism on sexual function may involve
central and peripheral processes.
Alcohol-induced peripheral neuropathy may result in
both erectile and ejaculatory
disorders. Schiavi outlined many of the psychological
factors that may also be present
such as preexisting personality problems,
mood disorder, and feelings of
inadequacy.35 He concluded that
“the reciprocal interaction
between drug intake and psychological factors
is so closely interwoven that it
is impossible to identify the nature
of this relation.”
Endocrine Abnormalities
“Erectile dysfunction of
exclusively endocrine origin is uncommon. . . In most cases
the primary effect of the
endocrine abnormality is loss of sexual interest.”12 The
authors
of the MMAS study arrived at a
similar conclusion.6” Of the 17 hormones
measured in
the MMAS, “only
dehydroepiandrosterone showed a strong correlation with impotence.”
Specifically, no correlations
were found between “impotence” and the following
hormones:
• Testosterone (total or free)
• Sex hormone binding globulin
(SHBG)
• Estrogens
• Prolactin
• Luteinizing hormone (LH)
• Follicle stimulating hormone (FSH)
When hormonal difficulties occur
in the context of erectile dysfunction, the more
common clinical abnormalities are
those that involve the hypothalamus-pituitarygonadal
axis and include: hypo- and
hypergonadotropic hypogonadism, hyperprolactinemia,
and hypo- and hyperthyroidism.41
(p. 85). The frequency of the association
of endocrine and erectile
problems depends on the age of the sample and the
Erectile dysfunction in all situations,
including the lack of nocturnal erections,
strongly suggests that a general medical
condition or substance use is the cause.5
|
clinical context of the
investigation (e.g., outpatient medical, urology, endocrine, or
sex therapy clinics), as well as
the nature of the sample.
When the particular association
of erection problems and hyperprolactinemia
(HPRL) was reviewed, the
observation was made that this was “often the first, and for
a long time the only symptom of
HPRL, an important point because in many cases the
cause is a pituitary tumor.”12
Buvat and Lemaire reviewed large
published series of endocrine abnormalities in
cases of erectile dysfunction and
when combining their own results with others
found an 8% prevalence for low
testosterone and 0.7% of prolactin levels greater
than 35 ng./ml.42
Aging
See “Sexual-developmenl History:
The Older Years” in Chapter 5.
Laboratory Investigation
When the history and physical
examination (see the “General Considerations” section
above in this chapter) leave
doubt about the origin of a patient’s erectile dysfunction,
the clinician must also consider
the use of laboratory tests.
The availability of orally
administered treatments for erectile dysfunction (for
example, sildenafil—see
“Treatment” below in this chapter) that appear to be easy to
use, often effective, and have
minimal side-effects may well have profound effects on
the process of evaluating
erectile dysfunction. The initial use of these medications by
a patient may, itself, become a
test, and in so doing may replace some other investigatory
procedures. Nothing, however,
should replace a careful clinical assessment and “when
there is suspicion of an organic
factor, one should rely (as well) on a combination of
investigations.”13
Laboratory investigation of
generalized erectile dysfunction chiefly entails examining
three body systems:
• Endocrine
• Vascular
• Neurological
Several diagnostic tests
involving these three systems have been developed. The criteria
used in considering which
diagnostic tests are appropriate for investigating generalized
erectile dysfunction on a primary
care basis are:
1. Usefulness
2. Low cost
3. Noninvasiveness
4. Low complexity
5. Availability
Endocrine Blood Tests
Endocrine and blood tests for
diabetes are probably the only procedures that fulfill the
criteria outlined immediately
above. Despite agreement on the endocrine disorders most
commonly associated with erection
difficulties,“. . . . there is disagreement on the specific
tests to be employed or the interpretation thereof”41 (p.
85). Many
suggest the need to measure
Testosterone (T) and Prolactin (PRL) in all
men with erection difficulty (PRL
can be abnormal when T is not). However,
others promote a more specific
policy. For example, Buvat and
Lemaire suggest that before age
50, T should be determined only in cases
of (accompanying) low sexual
desire and abnormal physical examination
but that after age 50 it
should be measured in all men, and that PRL should
be determined only in cases of
(accompanying) low sexual desire, gynecomastia,
and/or testosterone less than 4
ng/ml.42 These authors also direct clinicians to
repeat first results of abnormal
prolactin and testosterone determinations because of their
finding of normal second results
in 40% of their cases.
Apart from measuring total
testosterone, this hormone also can be determined in the
bioavailable form (BAT) and as
free testosterone (FT). BAT consists of FT and the fraction
that is bound to albumin41
(p. 76).
Conflicting opinions exist over
the need to also immediately test some or all of the
following other factors without
waiting for an abnormal T or PRL result:
• Follicle Stimulating Hormone
(FSH)
• Luteinizing Hormone (LH)
• Sex Hormone Binding Globulin
(SHBG)
• Thyroid function tests
Cost of testing and the nature of
the clinical context are two elements resulting in differences
of opinion. In the literature, it
seems assumed that these other factors would
be measured in the event of an
abnormal T or PRL level.
Tests for Diabetes
Fasting blood sugar (FBS) or
fasting plasma glucose (FPG) and/or glycosylated hemoglobin
(HgA1C)
is widely used as a screening test for diabetes. A positive test indicates
that a confirming diagnostic test
is warranted.43
Vascular Tests
Since the penis is, basically, a
vascular organ, vascular tests are often important elements
in the evaluation of erectile
difficulties, particularly when there is suspicion that
vascular elements may contribute
to the etiology. However, tests of
penile vascular function are
mostly invasive, costly, complex, difficult
to interpret, and have limited
availability. As such they are generally
conducted by urologists and not
recommended in primary care unless a
physician has special training.
Although vascular testing procedures
may not be recommended for use in
primary care, clinicians should be
aware of their potential
diagnostic benefits and limitations to determine
the need for urological
consultation.
Assessment of the penile response
to the intracavernous injection
(ICI) of vasoactive agents has
been found to be particularly useful in
considering vascular function.
While structural problems with cavernosal
arteries may explain a negative
response, anxiety can as well.44 “A
positive erectile response
implies normal veno-occlusive function.
These authors also direct clinicians to
repeat first results of abnormal prolactin
and testosterone determinations because
of their finding of normal second results
in 40% of their cases.
The most worrisome complication of ICI
is that of prolonged erection. After six
hours of continuous erection, there is
insufficient blood supply to the erectile
tissue. The corpora cavernosa must be
drained to decrease the intracavernosal
pressure and an adrenergic agonist
administered, injected intracavernously.
29 In
clinical practice, patients must
be told to contact a physician long
before six hours if their erection
persists.
|
Nonresponders bear a high
probability of a vascular origin with a predominance of
veno-occlusive insufficiency.”29
From a procedural viewpoint, the
most common substances used for intracavernosal
injections are papaverine,
papaverine-phentolamine mixture, or prostaglandin E1
(PGE1).
The most worrisome complication of ICI is that of prolonged erection. A
comparative study of these three
medications demonstrates that PGE1 had the highest
erection rate (75%) and lowest
prolonged erection rate (i.e., requiring “interruption”
[0.1%]).45 After
six hours of continuous erection, there is insufficient blood supply to
the erectile tissue. In this
situation, the corpora cavernosa need to be drained to
decrease the intracavernosal
pressure and an adrenergic agonist (e.g., 10 mg of adrenaline)
injected intracavernosly.29
In clinical practice, patients must be told to contact their
physician
long before six hours if their
erection persists.
Pharmacopenile Duplex
Ultrasonography (PPDU) provides “an estimate of penile
arterial inflow and venous
outflow . . . [and] . . . has become a first-line test to
define vascular [erectile
dysfunction]”29 It allows for accurate location of penile
arteries
and measurement of the diameter
of each artery and provides evidence of the thickness
and pulsatility of arterial
walls.12 In addition to assessment of the state of the
cavernosal
arteries, PPDU can locate
well-defined pathological conditions such as Peyronie’s
disease. The procedure for PPDU
involves the creation of an erection through
ICI (needed because the procedure
is unreliable when a penis is in the flaccid state)
and then simultaneously combining
ultrasound color imaging of the arteries to the
cavernosal bodies of the penis
with an analysis of blood flow patterns.
Nonspecific Tests: Nocturnal Penile Tumescence (NPT)
Any discussion of erectile
dysfunction assessment is incomplete without including
NPT testing, since it is so
widely used and so frequently included in the literature on
this subject. NPT is based on the
discovery that a period of sleep involves different
stages and that one of those
stages (REM) is associated with many body changes,
including the development of
erection in men (three or four times each night and
occupying about 20% of total
sleep time). It was assumed that erections that occur at
night and those which occur
during the day involve the same body mechanisms and
that by comparing sleep and
daytime erections, it would be possible to distinguish the
psychological or organic nature
of the etiology of erection dysfunction. Sleep erections
are considered to be unaffected
by waking psychosocial factors.
When used in-home, NPT testing
fulfills many of the primary care criteria previously
described insofar as it is
inexpensive, not extraordinarily complex to use, noninvasive,
and available. However, when done
in a sleep laboratory, NPT is the opposite
in that it is expensive,
cumbersome, and frequently unavailable in many geographic
areas. The chief doubt about NPT
is its usefulness.
When used in such a way as to
provide clearest interpretation, the test is performed
in a sleep laboratory with
measurement of other sleep parameters such as electroencephalograph
(EEG), respiration, and
electromyograph (EMG), and recordings are
made on at least two nights. The
purpose in monitoring other sleep parameters is the
detection of interference with
sleep or REM such as might happen with illness or
medication, which might result in
mistaken conclusions.
Because of the complexity,
expense, and difficulties with availability associated with
formal testing of NPT in a
hospital setting, three in-home procedures have been developed46
(p. 153):
1. The “stamp” test (a ring of
stamps placed around the base of a man’s penis)
2. Snap Gauge Band (one ring of a
thin plastic material containing three others that
break at three different levels
of tension as a penis enlarges)
3. Portable NPT monitoring
“Stamp” test results are
difficult to interpret because of such problems as falsepositive
findings due to accidental
tearing of the stamps for reasons other than an
erection, false-negative results
due to slippage, and lack of standardization. Snap Gauge
has similarly been found to be of
limited value. Both the stamp test and Snap Guage
provide information about changes
in circumference only, nothing about rigidity or
stiffness (a vital issue in the
assessment of erectile capacity for intercourse), and no
data concerning the number or
duration of tumescent episodes each night.
Portable monitors (e.g.,
Rigiscan) measure rigidity as well as the number and duration
of NPT episodes. Measurement of
rigidity has for some time been regularly
included in NPT testing (now
sometimes called NPTR with the “R” referring to rigidity).
Reasons include the finding of
substantial “interindividual differences in the
increase of circumference
associated with full erections and the recognition that maximal
increases in shaft circumference
did not indicate adequate rigidity.”47
As inviting as these in-home
methods of NPT testing might be, clinicians should be
fully aware of their considerable
limitations. It is suggested that this test “should be
used only as screening tools in
the context of a comprehensive medical and psychological
evaluation”46(p.
153).
Although the use of the Rigiscan
at-home is certainly less troublesome and expensive
than NPT in a sleep laboratory,
opinions differ concerning its usefulness. “Apart
from the lack of sleep data, it
is impossible to know if such devices have been misused,
manipulated, or otherwise
mishandled by the patient. Deliberate faking of results cannot
be excluded. . . .”12
Apart from issues of technology,
patient reliability, and cost, the utility of NPT
itself has been questioned. After
many years, the importace of NPT in the process of
evaluation of erectile
dysfunction remains unclear. So, too, is the question about the
equivalency of sleep and sexual
erections. Confusion abounds in findings that show, for
example, abnormal NPT
results in men who are not sexually dysfunctional in circumstances
such as aging,47
depression,48 and
diabetes.49 Conversely, normal NPT is reported in
men with multiple sclerosis who
have daytime erectile difficulties.50
Conclusions about the use of NPTR
when used in the clinical evaluation of erectile
dysfunction (in a sleep
laboratory or at home) are summarized Box 11-3.
Treatment
“Whether psychological issues are
co-determinates of the erectile problem or are reactive
to it is immaterial. A man’s
emotional reaction to his erectile failure may be such
that it serves to maintain the
erectile problem even when the initial physiological
causes are resolved . . . no
patient, even those with a clear organic impairment of
erectile capacity, can be
considered inappropriate for psychological as well as relevant
surgical or drug therapies for
his sexual problem”.54 For these reasons,
everything that
was written immediately above
about the treatment of situational erectile difficulties is
also applicable to the acquired
and generalized form.
Specific Treatments
Specific disorders and their
sexual symptoms are often (not always) therapeutically
responsive to specific
treatments. Therapy for hyper- and hypogonadotropic hypogonadism
and hyperprolactinemia have been
reviewed elsewhere41 (pp. 86-91). Details
concerning treatment will not be
discussed here, since primary care health professionals
likely seek consultation when
encountering such a patient.
Other specific disorders and
their sexual symptoms may not respond therapeutically
to specific treatment methods.
Diabetes is an example. Careful control of insulindependent
and probably
non-insulin-dependent diabetes mellitus will slow the onset
and delay the progression of
early vascular and neurologic complications, two body
systems that have been
particularly implicated in the etiology of erectile disorders in
this disease.55,56
Presumably, better control of diabetes would also delay the onset
and
slow the development of sexual
dysfunctions, including erectile difficulties. When
erectile dysfunction in specific
disorders such as diabetes do not respond to specific
treatment, nonspecific approaches
can be used.
Nonspecific Treatments
Dramatic developments in the
treatment of the acquired and generalized
form of erectile dysfunction have
been introduced in the past two
decades in the form of
intracavernosal injections, intraurethral medication,
erections devices, and
prostheses. As significant as these developments
have been, they might well be
overshadowed by the introduction
of new oral therapies. The
etiological and clinical heterogeneity
of the acquired and generalized
form of erection dysfunction will likely
Box 11-3
Nocturnal Penile Tumescence (NPT) Interpretation45-47
• Greatest benefit is to confirm a
situational (psychogenic) erectile disorder
• Evidence of significant erectile activity
during a single night may be sufficient to demonstrate
the potential for normal functioning
• Repeated demonstration of insufficient
rigidity in an otherwise normal male is not necessarily
pathological
• Abnormal findings may coexist with normal
daytime function in older men, men with
diabetes, and nondepresssed men with a
recent history of major depression
• May not be helpful in neurological
disease in proving waking erectile capacity
• Should be conducted only in a sleep
(versus home) laboratory when certain factors
coexist (e.g., manual dexterity problems,
dementia, malingering, medico-legal assessment,
and sleep disorder)
As a result of factors such as the ease of
administration, sildenafil (and other
orally administered substances currently
being tested) will likely result in a
substantial
shift in the treatment of men
with erectile difficulties away from
specialists
and toward physicians in primary
care.
|
necessitate the continued use of
several treatment approaches. Not everyone will benefit
from the new oral therapies. For
this reason, the oral therapies and many of the
other currently used treatment
approaches are discussed below.
Oral Therapies
Sildenafil (Viagra),
is a new oral treatment that may be a critical advancement in the care
of men with erectile difficulties
(Box 11-4).
As a result of factors such as
the ease of administration, sildenafil (and other orally
administered substances currently
being tested) will likely result in a substantial shift
in the treatment of men with
erectile difficulties away from specialists and toward
physicians in primary care.
Sildenafil demonstrated in initial trials to be well tolerated
and “effective in improving erectile
activity in patients with male erectile dysfunction
for which there is no established
organic cause.”57
Box 11-4
Sildenafil (Viagra) Highlights 62, product monograph
• MECHANISM OF ACTION: Sexual stimulation
results in release of nitric oxide (NO);
NO stimulates the production of cyclic
guanosine monophosphate (cGMP), which
relaxes smooth muscle and promotes the
inflow of blood into the corpus cavernosum;
phosphodiesterase type 5 (PDE5) is an
enzyme that inhibits cGMP; sildenafil inhibits
PDE5 (and therefore causes increased levels
of cGMP)
• PLASMA CONCENTRATION LEVELS: Maximal
within one hour after oral administration
• HALF-LIFE of 3 to 5 hours
• ADMINISTRATION: Taken on an “as needed”
basis about one hour (0.5 to 4 hours)
before sexual activity
• FREQUENCY OF USE: Maximum recommendation
is once/day
• STARTING DOSE: Recommendation is 50 mg
but can vary from 25 to 100 mg,
depending on efficacy
• EFFICACY: Eighty percent of men with
erectile dysfunction (ED) taking 50 mg will
have sufficiently firm erections for
intercourse
• ASSOCIATED SEXUAL STIMULATION: Necessary
• ETIOLOGY OF ED: Similar benefit
regardless of etiology
• OTHER SEXUAL BENEFITS: Orgasmic function,
intercourse satisfaction, and overall
satisfaction but not for sexual desire
• PARTNERS: Verify erectile improvement and
report significant enhancement of their
satisfaction
• SIDE EFFECTS: Increase with increasing
dose and include (at 50 mg): headache (21%),
flushing (27%), dyspepsia (11%), rhinitis
(3%), and visual disturbance (6%; change in the
perception of color hue or brightness). No
priapism reported
• CONTRAINDICATION: Potentiates hypotensive
effects of organic nitrates. Therefore,
not to be taken with organic nitrates in
any form, including nitroglycerin
|
As described above (see
“Mechanism of Erection” in this chapter), relaxation of
smooth muscle is an essential
aspect of the development of an erection. This relaxation
is mediated by nitric oxide via
cyclic guanosine monophosphate (cGMP).59 Cyclic
nucleotide phosphodiesterase
(PDE) isozymes hydrolyse cGMP. It was reasoned that
an inhibitor of PDE would
therefore enhance the action of nitric oxide/cGMP on
penile erectile activity.
Sildenafil is such an inhibiting agent.59 It
is described as the first
representative of a new class of
agents: an enzyme inhibitor (type 5 cyclic guanosine
monophosphate-specific
phosphodiesterase isozyme) that results in the relaxation of
corpus cavernosum smooth muscle
cells and thereby enhances penile erection in
response to sexual stimuli.60
An initial report on sildenafil
involved 12 subjects and was conducted in two phases:
(1) a single dose in a laboratory
and (2) once-daily doses at home for seven days, 1
to 2 hours before sexual activity
was likely to occur.57 Both phases were placebocontrolled,
double-blind, and involved a
cross-over design. The first included use of
the drug at three different doses
and measured erectile response to visual sexual stimulation
using subject-chosen explicit
videos and magazines. In the second phase, subjects
kept a diary and graded their
erections. Results from the first phase demonstrated
a significant difference in
penile rigidity between all three doses of sildenafil and placebo,
with the difference being more
substantial as the dose increased. The in-home
phase showed that higher quality
erections occurred more often when men were on
the drug. Adverse events were
described as “mild and transient.”
Another report on sildenafil was
conducted on 250 patients with erectile dysfunction
of “predominantly no known
organic cause.”61 Patients previously were involved
in an open dose study and were
randomized to receive their optimum dose of the
medication or placebo. They were
asked to compare their erections in the present
study to those they experienced
in the open trial. Of those given sildenafil, 59%
reported no change, and of those
receiving placebo, 72% reported their erections as
“much worse.” The authors
concluded that sildenafil must be continued
for the erectile improvement to
be maintained.
The most complete report on oral
sildenafil (as of Spring 1998) was
published in the New England
Journal of Medicine (NEJM). It involved
a total of 861 men with erectile
dysfunction described as organic, psychogenic
or mixed.62 Two
studies were conducted: (1) a dose-response
study on 532 men treated with 25,
50, 100 mg or placebo and (2) a
dose-escalation study involving
329 different men treated initially with
50 mg or placebo and subsequently
with one half or twice the amount
of the original dosage, depending
on efficacy and tolerance. These
studies were performed in a
natural environment and therefore relied
on the subjects’ reports of
efficacy.
In the first study
(dose-response) in the NEJM report, increasing doses of sildenafil
were associated with significantly
increased “frequency of penetration” and maintenance
of erections after entry
(p<0.001). Interestingly, the cause of the erection difficulty did
not affect the outcome. In the
second study (dose-escalation), improvement of the same
two measures were significantly
better for sildenafil compared to placebo (p<0.001), as
were several other measures,
including “overall satisfaction.” (However, in this same
study, sexual desire scores were
not different in the two groups). In the dose-response
In a dose-response study, the frequency
of erections sufficiently firm for
intercourse
to occur was 72%, 80%, and 85%
for doses of 25 mg, 50 mg, and 100
mg, respectively (versus 50% for the
placebo group; p<0.001). In the
doseescalation
study, 69% of attempts at
intercourse (versus 22% for the placebo
group) were successful (p<0.001).
|
study, the frequency of erections
sufficiently firm for intercourse to occur was 72%,
80%, and 85% for doses of 25 mg,
50 mg, and 100 mg, respectively (versus 50% for the
placebo group; (p<0.001). In
the dose-escalation study, 69% of attempts at intercourse
(versus 22% for the placebo
group) were successful (p<0.001).
Yohimbine is
one of the more widely used and studied oral agents used recently in the
treatment of erectile dysfunction.
It is an alkaloid derivative that is found in the bark
of the yohimbine tree and has a
long-standing reputation as an aphrodisiac.63 Part
of
the attractiveness of yohimbine
is the “benign side effect profile”33 (p. 123).
Pharmacologically,
yohimbine is a preferential
presynaptic alpha 2 antagonist. The dose ranges
from 2 to 6 mg three times per
day, and has shown to have a positive effect on sexual
behavior in animals).64
However, a review of the outcome of several studies of men
with erectile dysfunction
indicates that while yohimbine may have the capacity to
affect sexual desire and
performance in some subjects, “results have been far from conclusive
[since] more than half of all
patients studied thus far have shown little or no
benefit from the drug.”63
A meta-analysis of studies of the effect of yohimbine in men
with erection difficulties
concluded the opposite, namely, that it was consistently helpful
compared to placebo.65
It may be that the heterogeneity of men with erection
difficulties that is evident in
many studies has disguised a beneficial effect of this
substance in a particular
subpopulation. One hypothesis suggests that men with a
“nonorganic
etiology” might derive a greater
benefit than other men.64
Androgens often
have been administered to men with erection difficulties, frequently
without establishing the presence
of an endocrinopathy. Studies of androgen treatment
in erectile dysfunction that
included hormonal assessments strongly suggest that it “is
of little value in eugonadal
males”40 (p. 91). The hazards of androgen therapy in
this
situation have not always been
considered. Given the fact that erectile dysfunction and
prostate cancer become more
evident with increasing age, clinicians need to be especially
concerned about the potentially
negative effect of androgens (even on a trial
basis) on the prostate gland (see
Etiology, “Endocrine Abnormalities” above in this
chapter).
Intracavernosal Injections (ICI)
Injection of medications directly
into one of the corpora cavernosa of a man’s penis as
a treatment of erectile
dysfunction became an accepted and widely used treatment
method in the 1980s. It would not
be surprising to see this approach greatly diminish
in popularity with the advent of
an efficacious and safe oral medication.
Three substances are currently
used for ICI:
• Papaverine hydrochloride
• Phentolamine mesylate
• Prostaglandin E1
(PGE1)
Papaverine has been used alone or
in combination with phentolamine; PGE1 has been
used alone or together with
papaverine and phentolamine as Trimix. One formulation
of PGE1 is
alprostadil. The subject of ICI treatment is thoroughly reviewed elsewhere.
66,67
Dosages are generally titrated to
the response of the patient. PGE1 alone is
the substance most commonly used
by urologists and the dose is typically in the range
of 1 to 40 μg.67
Smaller doses of medications used in ICI are generally required in
instances of neurogenic (and
“psychogenic”) erectile dysfunction.
ICI seems most efficacious in the
context of a neurological deficit (e.g., spinal cord
injury) and least helpful in men
who have severe corporal veno-occlusive dysfunction
and/or arterial insufficiency.
Contraindications include poor manual dexterity, morbid
obesity, and anticoagulant
therapy.67 Injection usually results in a partial
erection
within minutes and the addition
of sexual stimulation usually increases the enlargement.
68 Patient’s are taught the
technique of injection (usually by a urologist or nurseeducator)
and “observed while
self-injecting so that the physician has an opportunity
to advise and correct his
technique.” Patients then inject themselves at home.67 One
side effect, namely, prolonged
erection (defined as more than four hours), requires
immediate medical attention. The
frequency of prolonged erection (priapism) and
other side effects depends on the
medication used. Side effects include the following:
• Fibrotic nodules (more with
papaverine and/or phentolamine)
• Pain (about 10% to 34% with PGE1
alone)
• Infection
• Bruising
• Liver function abnormalities
• Vasovagal episodes
Prolonged erections appear to
more common with papaverine alone (10% of patients)
than PGE1 alone
(2% of patients). The incidence of priapism seems to be less with the
mixture of
papaverine-phentolamine-PGE1.67
Priapism rates for home injections are
considerably less (0.3%) than
in-office trial injections. When priapism occurs, emergency
intervention is required, and
most cases resulting from papaverine and/or
phentolamine respond to
aspiration alone, or in combination with intracorporal installation
of a diluted alpha-adrenergic
receptor agonist such as epinephrine (limited to
less than 15 μg
at intervals of more than five minutes to avoid systemic side
effects).69
Fibrotic plaques are reported to
be less common with PGE1 than with
papaverine
and/or phentolamine, and there
have been no reports of liver disease with either of
these substances or with PGE1
despite abnormalities on liver function testing.67
Pain
during injection is commonly
reported by men using PGE1 (75% in
one study) but
pain is infrequent with
papaverine and/or phentolamine.67
The impact of ICI on patients and
their partners was studied and beneficial changes
were described in each,
particularly in the areas of self-esteem, sexual desire, frequency,
and satisfaction.66,67
Although ICI is considered safe
and reliable, many patients do not continue using
it in the short-run for several
reasons, including67:
1. The feeling that it was
unnatural
2. Concerns about side effects
3. Lack of a regular partner
4. Fear of being belittled by the
partner
In addition to immediate issues,
there is a surprisingly high (50%) drop out rate at 12
month follow-up. Reasons given
include loss of efficacy and loss of interest. The high
drop out rate suggests the need
for a careful initial evaluation of the motivation of the
patient and partner and
willingness to accept ICI on the part of both.
Transurethral Alprostadil
Alprostadil is a synthetic
compound identical to PGE1. A
transurethral method of delivering
this medication was developed as
an alternative to intracavernosal injections. With
medicated urethral system for
erection (MUSE), a proprietary drug delivery system, the
medication is put into a tiny
pellet and deposited into the end of the urethra with an
applicator. A man urinates before
insertion of the applicator to lubricate his urethra.
Route of administration of any
medication may result in different side effects even
though the substance might be the
same. In the form of intracavernosal injections,
alprostadil enters directly into
the corpus cavernosum of the penis. When given transurethrally,
the medication is absorbed from
the urethral mucosa, enters the body’s
blood stream, and then is
returned to the penis.
In a double-blind and
placebo-controlled study, 1511 men aged 27 to 88 with “chronic
erectile dysfunction from various
organic causes” were treated with transurethral alprostadil.
70 To determine maximal
penile response, subjects were given the opportunity to
use up to four alternative doses
of the drug: 125, 250,500, or 1000 μg. The
996 men
who responded in a clinic setting
were then randomly assigned to the selected dose or
placebo. Eighty-eight percent of
the men completed the three month course of treatment.
Significantly more men in the
alprostadil group (65%) reported having intercourse
at least once and the medication
was significantly more effective than placebo
regardless of age or the cause of
the erectile dysfunction.
The most common side effect of
transurethral alprostadil was penile pain (reported
by 33% of the men) but was
considered mild and resulted in only 20% of the men
leaving the study.70
Other side effects include mild urethral trauma (5%), dizziness
(2%), and urinary tract
infections (“rare”).
Transurethral alprostadil is particularly
advantageous in primary care. For the physician
the procedure is greatly
simplified (compared to ICI) in that the medication is
self-administered and does not
require an in-office training procedure. From the
patient’s perspective, the
process is less complex to learn and to use at home and free
of the potentially serious side
effects of priapism and fibrosis associated with ICI.
Vacuum Erection Devices
Vacuum erection devices (VEDs)
are also called vacuum constriction, and external
vacuum, devices (information
available through Imagyn Technologies at
1-800-344-9688). Like
intracavernosal injections, the use of VEDs may diminish considerably
with the advent of a safe and
effective oral treatment for erectile dysfunction.
However, for the foreseeable
future, VEDs are likely to remain in the armamentarium
of health professionals who treat
men with erectile dysfunction. The need is exemplified,
for example, in men for whom a
physical approach is recommended but who
strongly prefer not to use any kind
of drugs for an ailment that could be treated in a
nonpharmacological manner. The
subject of VEDs is reviewed in detail elsewhere.66
When first introduced in the
early 1980s, “the concept [of VEDs] seemed difficult
for physicians to accept. In an
era of high technology, perhaps the low technology and
simplicity of vacuum devices are
disarming and provoke rejection”66 (p. 297).
Precisely
because they are “low tech,”
safe, and efficacious, VEDs are likely to remain of particular
interest to primary care clinicians.
The mechanism of action is
fundamentally the same for the various VEDs that exist.
Procedures are as follows:
• A cylinder is placed over a
man’s flaccid penis and pressed firmly against
his body to create an airtight
seal
• Air is pumped out of the
cylinder to create a vacuum
• Blood is, in the process, drawn
into his penis
• After an erection exists, a
tension band is transferred from the VED to
the base of the man’s penis
• A vacuum release valve is then
opened and the cylinder is removed
VED-induced erections are
passively created by suction and venous stasis that results
from constriction, in contrast to
erections produced naturally (and by ICI), which are
actively created by
neurotransmitters and relaxation of corpora smooth muscle. Several
studies demonstrate that 90% of
men who have “organic,” “mixed,” and “psychogenic”
erection dysfunction and use this
system are able to have sufficiently firm erections for
the purpose of intercourse.66
The most common side effects
reported with VEDs are hematoma and petechiae
(8% to 50%).66
These are generally not considered serious and resolve without
medical
intervention. Other side effects
include the following:
• Pain
• Numbness of the penis
• Pulling of scrotal tissue into
the cylinder
• Blocked and painful ejaculation
Patient acceptance is estimated
at 80% to 95%. The reasons for discontinuing the
use of a VED include the
following:
• Mechanical difficulty
• Failure to produce an adequate
erection
• Feeling that the device is
cumbersome
• A sense that the erection is
artificial
There are three
contraindications: men with Peyronie’s Disease,
concurrent blood dyscrasia or use
of anticoagulants, and poor manual
dexterity (which can be overcome
by the use of a battery operated
device).
Table 11-1 summarizes comparisons
between VEDs and ICI. Since they are both
equally efficacious and have a
positive effect on patients, “the critical discriminations
need to be made on the basis of
cost, potential side effects, patient acceptance, and
aesthetic preferences of the man
or couple”66 (p. 304).
Penile Prostheses
The use of prostheses (or
implants) in the treatment of men with erectile dysfunction
is generally considered “a last
resort,” since surgery involves the destruction of structures
which are otherwise normally
involved in the erectile process. The irreversibility
The irreversibility of prosthesis
implantation
limits its use given the rapid progress
in the development of more benign
approaches to the treatment of this
disorder.
|
of prosthesis implantation limits
its use given the rapid progress in the development of
more benign approaches to the
treatment of this disorder. The subject of prostheses
has been thoroughly reviewed
elsewhere.71
Implants have been used since the
early 1950s and now exist in a variety of forms:
semirigid silicone only;
semirigid, silicone interior; and inflatable.71 “Most
operating
rooms stock one type of semirigid
device and the inflatable prosthesis used most
often by the implanting surgeons”
(p. 270). Some factors that influence the choice of
device include: cost,
availability, esthetics, and manual dexterity (to use the inflatable
type) (p. 271).
In a follow-up examination on the
satisfaction of patients (n = 52) and their partners
(n = 22), which involved interviewing
the two people separately and had a
response rate of 72%, the kind of
device implanted made little difference to the men.
However, the patient’s partner
preferred inflatable implants.72 All
except four had
intercourse more than
“infrequently.” Almost 80% of the men said they would undergo
the operation again but only 60%
of the partners said that they had no hesitations.
The goal of treatment with penile
prostheses can vary greatly and depends to a
large extent on the perspective
of the discipline of the person stating an opinion. Some
urologists focus specifically on
the issue of erection, whereas mental health professionals
and sex therapists concentrate
more broadly on sexual satisfaction of the two partners.
One follow-up study did not resolve
the conflict (but leaned more toward the
view of sex therapists), since it
demonstrated that the greatest benefit is the sense of
“restored manhood.” “The feeling
of being capable of coitus, was reported by many of
the men in the study as a prime benefit
of surgery” (italics added)71 (p. 273).
Screening
issues have been identified to
detect patients for whom penile prosthesis implantation
is planned but who might benefit
also from preventive counseling.73 These
include the
following factors:
• Concern about the importance of
penile size in sexual activity
• Disinterest in foreplay
• Low sexual desire in either
partner
• Premature ejaculation
• Untreated vaginal atrophy in
the woman
Indications for Referral for Consultation or Continuing
Care by a Specialist
The treatment of solo men, or
couples, in which the man has an acquired and generalized
form of erectile dysfunction
requires attention to both physical and psychological
etiological issues. The more the
etiologies are known, the more specific will be the
treatment, as well as the kind of
health professional needed to provide the necessary
form of care. Referral for
medical specialist consultation may be useful in, for example,
the following specific and
defined circumstances:
• Endocrine disorders
• Diabetes
• Cardiovascular disorders
(including hypertension)
• Major depression
Referral to a urologist for
continuing care might be beneficial in instances of “venous
leak.”
When complex, expensive, or
physically invasive diagnostic procedures are necessary
to clarify the etiology,
consultation with a urologist who is knowledgeable about
erectile disorders is required.
Buvat reminded clinicians of “ . . . Cochran’s aphorism:
‘before doing a test, decide what
to do if it is (a) positive and (b) negative. If both
answers are the same, don’t do
the test.”12
When the etiology is unknown (or
the etiology known but not responsive to specific
therapy), treatment is
nonspecific. The advent of safe and effective oral therapies
will likely result in many more men
with erectile dysfunction being identified and
cared for on a primary care basis
than at present. However, liberal use should be made
of other health professionals
(especially urologists and sex therapists) when cases are
treatment-resistant (for the purpose
of consultation and possible implementation of
other nonspecific treatment
approaches).
Summary
Impotence is
a term that is widely used and accepted but falls short of being helpful for
two reasons: (l) confusion, since
several conditions are grouped in the same category
and (2) even more confusion,
since the disorders have nothing to do with power (the
origin of the word “potency”).
The prevalence of erectile
disorders is 40% of men at age 40 and 66% at age 70.
The resources needed to treat
this widespread problem are substantial and will become
even more substantial as the
aging population increases.
In the same way that different
cardiac disorders manifest in similar ways despite
having several origins, so do
erectile disorders. While the chief manifestation of an
erectile disorder is a soft penis
rather than a hard one, the pattern of erection function
matters when considering etiology
(“psychogenic” and “organic”) and treatment. An
erectile problem that is
generalized (exists in all situations: with a partner, in the morning,
and with masturbation) suggests a
different etiological and treatment direction
than one that is situational
(erections are unimpaired in some situations). Likewise, it
matters if erection problems have
always existed, since the man has been sexually
involved with others (lifelong)
or developed more recently (acquired).
Causes of erectile disorders
(often more than one) include the following:
• Medical disorders (endocrine,
cardiovascular, neurological)
• Drugs
• Elevated blood lipids
• Cigarette smoking
• Psychiatric disorders
• Relationship problems
• Anxiety
In any investigation of an
erectile disorder, history-taking is essential, a physical
examination is necessary
(although the yield is low), and laboratory tests are required
if the pattern of erectile
dysfunction even hints at being generalized.
Treatment of erectile disorders
are sometimes specific to the etiology (e.g., replacing
a hormone that exists in
insufficient amounts) and sometimes nonspecific, for
example, oral medications
(sildenafil [Viagra], psychotherapy, or intracavernosal injections.
Counseling intervention ranges
from being central (sex therapy) to being an
adjunct (e.g., information about
the use of vacuum erection devices).
The prevalence of erectile disorders
makes primary care health professionals central
to the care of men (and couples)
with this disorder. Their task will likely be made
easier by the introduction of
safe and effective oral therapies. However, even with the
advent of new forms of care there
still will be treatment-resistant patients and couples,
and in those instances, liberal
use should be made of other approaches and specialists.
Postscript
When a patient takes no action
after treatment suggestions are made for erectile difficulties,
clinicians should not necessarily
be surprised or discouraged.
A 57-year-old divorced computer analyst was
seen because of long-standing (about
ten years) erectile difficulties that
appear when alone in masturbation and on the
occasional times he is sexually active with
a partner. He experienced a myocardial
infarction four years before the referral.
He lived alone for 25 years after a marriage
that lasted three years. The longest
relationship he had with a woman since then
(he was not romantically or sexually
interested in men) was four months and that
was about 20 years before. Since then he
had a few dates but none in the previous
ten years because he felt that women would
expect him to do what he felt was not
possible, that is, to sexually “perform.”
Discontented with the suggestions made at
the end of a thorough assessment, he
insisted on special diagnostic vascular procedures
about which he had read. He was unwilling
to consider oral medications,
intracavernosal injections, or VEDs and was
angry about the suggestion of psychiatric
care as part of a treatment “package.” He
did not appear again after two visits
and canceled his last appointment.
A survey of men assessed for
erectile problems in a urology clinic found that two years
later over half had not followed
up on recommendations.74 Sexual
and nonsexual reasons
may have existed. A strong desire
for return of erectile capability may not be
durable after the discovery that
treatment entails significant psychological and/or
physical effort and discomfort.
In addition, some men are quite resistant to the notion
that the explanation for problems
with the function of their genitalia may, in fact, lie
elsewhere (e.g., the problems may
be an expression of intimacy difficulties [see Appendix
II]).
REFERENCES
1. Rosen RC, Leiblum SR: Erectile disorders:
an overview of historical trends and clinical
perspectives. In Rosen RC, Leiblum SR
(editors): Erectile disorders: assessment and treatment,
New York, 1992, Guildford Press, pp. 3-26.
2. Elliott ML: The use of “impotence” and
“frigidity”: why has “impotence” survived, J Sex
Marital Ther 11:51-56,
1985.
3. Impotence. NIH Consensus Statement
10:1-31, 1992
4. Lue TF, Tanagho EA: Functional anatomy and
mechanism of penile erection. In Tanagho
EA, Lue TF, McClure RD (editors): Contemporary
management of impotence and infertility.
Baltimore,1988, Williams & Wilkins.
5. Diagnostic and Statistical Manual of
Mental Disorders, ed 4, Primary Care Version, Washington,
1995, American Psychiatric Association.
6. Feldman HA et al: Impotence and its
medical and psychosocial correlates: results of the
Massachusetts male aging study, J Urology 151:54-61,1994.
7. Rosen RC, Leiblum SR: Erectile disorders:
an overview of historical trends and clinical
perspectives. In Rosen RC, Leiblum SR
(editors): Erectile disorders: assessment and treatment,
1992, The Guilford Press, pp. 3-26.
8. Spector IP, Carey MP: Incidence and
prevalence of the sexual dysfunctions, Arch Sex
Behav 19:389-408,
1990.
9. Masters WH, Johnson VE: Human sexual
inadequacy, 1970, Little, Brown and Company.
10. Althof SE, Seftel AD: The evaluation and
management of erectile dysfunction, Psych Clin
N Am 18:171,1995.
11. LoPiccolo J: Postmodern sex therapy for
erectile failure. In Rosen RC, Leiblum SR
(editors): Erectile disorders: assessment
and management, New York, 1992, The Guilford Press,
pp. 171-197.
12. Buvat J et al: Recent developments in the
clinical assessment and diagnosis of erectile
dysfunction, Ann Rev Sex Res 1:265-308,1990.
13. O’Leary MP et al: A brief male sexual
function inventory for urology, Urol 46:697-706,
1995.
14. Schover LR, Jensen SB: Sexuality and
chronic illness: a comprehensive approach, New York, 1988,
The Guilford Press.
15. Slag MF et al: Impotence in medical
clinic outpatients, JAMA 249:1736-1740,
1983.
16. Rosen RC, Leiblum SR, Spector IP:
Psychologically based treatment for male erectile
disorder: a cognitive-interpersonal model, J
Sex Marital Ther 20:67-85, 1994.
17. Levine SB: Intrapsychic and interpersonal
aspects of impotence: psychogenic erectile
dysfunction. In Rosen RC, Leiblum SR
(editors): Erectile disorders: assessment and treatment,
1992, The Guilford Press, pp. 198-225.
18. Masters WH, Johnson VE: Human sexual
response, Boston, 1966, Little, Brown and
Company.
19. Althof SE: Psychogenic impotence:
treatment of men and couples. In Leiblum SR, Rosen
RC (editors): Principles and Practice of
Sex Therapy: Update for the 1990s, ed 2, New York, 1989,
The Guilford Press, pp. 237-265.
20. Zilbergeld B: The new male sexuality,
New York, 1992, Bantam Books.
21. Goldman A, Carroll JL: Educational
intervention as an adjunct to treatment of erectile
dysfunction in older couples, J Sex
Marital Ther 16:127-141,1990
22. Cranston-Cuebas MA, Barlow DH: Cognitive
and effective contributions to sexual
functioning, Ann Rev Sex Res 1:119-161,
1990.
23. Turner LA et al: Self-injection of
papaverine and phentolamine in the treatment of
psychogenic impotence, J Sex Marital Ther 15(3):163-176,
1989.
24. De Amicis LA et al: Clinical follow-up of
couples treated for sexual dysfunction, Arch Sex
Behav 14:467-489,
1985.
25. Hawton K et al: Long-term outcome of sex
therapy, Behav Res Ther 24:665-675, 1986.
26. Schiavi RC et al: Diabetes mellitus and
male sexual function, Diabetologia 36:745-751, 1993.
27. Report of the expert committee on the
diagnosis and classification of diabetes mellitus,
Diabetes Care 20:1183-1197,
1997.
28. Nofzinger EA et al: Results of nocturnal
penile tumescence studies are abnormal in
sexually functional diabetic men, Arch
Internal Med 152:114-118, 1992.
29. Meulemann EJ, Diemont WL: Investigation
of erectile dysfunction: diagnostic testing for
vascular factors in erectile dysfunction, Urol
Clin N Am 22:803-819, 1995.
30. Virag R, Bouilly P, Frydman D: Is
impotence an arterial disorder? Lancet 8422:181-184,
1985.
31. Condra M et al: Prevalence and
significance of tobacco smoking in impotence, Urol
27:495-498, 1986.
32. Rosen MP et al: Cigarette smoking: an
independent risk factor for atherosclerosis in the
hypogastric-cavernosus arterial bed of men
with arteriogenic impotence, J Urol
145:759-763, 1991.
33. Crenshaw TL, Goldberg JP: Sexual
pharmacology: drugs that affect sexual function, New York,
1996, W.W. Norton & Company, Inc.
34. Segraves RT, Segraves KB: Aging and drug
effects on male sexuality. In Rosen RC,
Leiblum SR (editors): Erectile disorders:
assessment and treatment, New York, 1992, The Guilford
Press, pp. 96-138.
35. Schiavi RC: Chronic alcoholism and male
sexual dysfunction, J Sex Marital Ther 16:23-33,
1990.
36. Lemere F, Smith JW: Alcohol-induced
sexual impotence, Am J Psychiatry 130:212-213, 1973.
37. Whalley LJ: Sexual adjustment of male
alcoholics, Acta Psychiatr Scand 58:281-298, 1978.
38. Jensen SB: Sexual function and
dysfunction in younger married alcoholics: a comparative
study, Acta Psychiatr Scand 69:543-549,
1984.
39. Snyder S, Karacan I: Effects of chronic
alcoholism on nocturnal penile tumescence,
Psychosom Med 43:423-429,
1981.
40. Bannister P, Lowowsky MS: Ethanol and
hypogonadism, Alcohol Alcoholism 22:213-217,
1987.
41. Davidson JM, Rosen RC: Hormonal
determinents of erectile function. In Rosen RC,
Leiblum SR (editors): Erectile disorders:
assessment and treatment, New York, 1992, The Guilford
Press, pp. 72-95.
42. Buvat J, Lemaire A: Endocrine screening
in 1,022 men with erectile dysfunction: clinical
significance and cost-effective strategy, J
Urol 158:1764-1767, 1997.
43. WHO Expert Committee on Diabetes
Mellitus: World Health Organization Technical Report
Series 646,
Geneva, 1980 World Health Organization.
44. Buvat J et al: Is intracavernous
injection of papaverine a reliable screening test for
vascular impotence? J Urol 135:476-478,
1986.
45. Porst H: Diagnotic use and side-effects
of vasoactive drugs—a report on over 2100
patients with erectile failure, Int J
Impotence Res 2(2):222-223,1990.
46. Schiavi RC: Laboratory methods for
evaluating erectile dysfunction. In Rosen RC,
Leiblum SR (editors): Erectile disorders:
assessment and treatment. New York,1992, The Guilford
Press, pp. 141-170.
47. Schiavi RC et al: Healthy aging and male
sexual function, Am J Psychiatry 147:766-771,
1990.
48. Nofzinger EA et al: Sexual function in
depressed men, Arch Gen Psychiatry 50:24-30, 1993.
49. Nofzinger EA et al: Results of nocturnal
penile tumescence studies are abnormal in
sexually functional diabetic men, Arch
Intern Med 152:114-118, 1992.
50. Kirkeby HJ et al. Erectile dysfunction in
multiple sclerosis, Neurology 38,1366-1371, 1988.
51. Kirkeby HJ, Andersen AJ, Poulsen EU:
Nocturnal penile tumescence and rigidity:
translation of data obtained from normal
males, Int J Impotence Res 1:115-125, 1989.
52. Levine LA, Carroll RA: Nocturnal penile tumescence
and rigidity in men without
complaints of erectile dysfunction using a
new quantitative analysis software, J Urol
152:1103-1107, 1994.
53. Levine LA, Lenting EL: Use of nocturnal
penile tumescence and rigidity in the evaluation
of male erectile dysfunction, Urol Clin N
Am 22:775-788, 1995.
54. Schreiner-Engel P: Therapy of psychogenic
erectile disorders, Sex Disability 4:115-122,
1981.
55. The Diabetes Control and Complications
Trial Research Group. The effect of intensive
treatment of diabetes on the development and
progression of long-term complications in
insulin-dependent diabetes mellitus, N
Engl J Med 329:977-986, 1993.
56. McCullough DK et al: The prevalence of
diabetic impotence, Diabetologia
18:279-283,1990.
57. Boolell M et al: Sildenafil, a novel
effective oral therapy for male erectile dysfunction, Brit
J Urology 78:257-261,
1996.
58. Lue T: Editorial Comment, J Urol 157:2021,
1997.
59. Boolell M et al: Sildenafil: an orally
active type 5 cyclic GMP-specific phosphodiesterase
inhibitor for the treatment of penile
erectile dysfunction, Int J Impotence Res 8:47-52, 1996.
60. Wicker P: Phosphodiesterase inhibitors
and male erectile dysfunction. Presented at the
1997 Annual Meeting of the Society for Sex
Therapy and Research, Chicago, 1997.
61. Virag R et al: (Pfizer Central Reseach,
UK): Sildenafil (Viagra), a new oral treatment for
erectile dysfunction (editor): an 8 week
double-blind, placebo-controlled parallel group
study. Presented at the VII World Meeting of
the International Society for Impotence
Research, San Francisco, 1996.
62. Goldstein I et al: Oral sildenafil in the
treatment of xerectile dysfunction, N Engl J Med
338:1397-1404, 1998.
63. Rosen RC, Ashton AK: Prosexual drugs:
empirical status of the “new aphrodesiacs,” Arch
Sex Behav 22:521-543,
1993.
64. Mann K et al: Effects of Yohimbine on
sexual experiences and nocturnal penile
tumescence and rigidity in erectile
dysfunction, Arch Sex Behav 25:1-16, 1996.
65. Carey MP, Johnson BT: Effectiveness of
Yohimbine in the treatment of erectile disorder:
four meta-analytic integrations, Arch Sex
Behav 25:341-360, 1996.
66. Althof SE, Turner LA: Self-injection
therapy and external vacuum devices in the
treatment of erectile dysfunction. In Rosen
RC, Leiblum SR (editors): Erectile disorders:
assessment and treatment,
New York, 1992, The Guilford Press, pp. 283-309.
67. Fallon B: Intracavernous injection
therapy for male erectile dysfunction, Urol Clin N Am
22:833-845, 1995.
68. Donatucci CF, Lue TF: The combined
intracavernous injection and stimulation test:
diagnostic accuracy, J Urol 148:61-62,
1992.
69. Lue TF et al: Priapism: a refined
approach to diagnosis and treatment, J Urol
166:104-108, 1986.
70. Padman-Nathan H: Treatment of men with
erectile dysfunction with transurethral
alprostadil, N Eng J Med 336:1-7,1997.
71. Melman A, Tiefer L: Surgery for erectile
disorders: operative procedures and
psychological issues. In Rosen RC, Lieblum SR
(editors): Erectile disorders: assessment and
treatment.
New York, 1992, The Guilford Press, pp. 255-282.
72. Pederson B et al: Evaluation of patients
and partners 1 to 4 years after penile prosthesis
surgery, J Urol 139:956-958, 1988.
73. Schover LR: Sex therapy for the penile
prosthesis recipient. Urol Clin N Am 16:91-98,
1989.
74. Tiefer L, Melman A: Adherence to
recommendations and improvement over time in men
with erectile dysfunction, Arch Sex Behav 16:301-308,
1987.