CHAPTER 10
Ejaculation/Orgasm Disorders
Three
disorders of ejaculation/orgasm are most common in primary care: Premature
Ejaculation [PE], Delayed
Ejaculation/ Orgasm [DE/O], and Retrograde Ejaculation
[RE]. Three others are found
infrequently: Anejaculation, Painful Ejaculation, and
Anorgasmic Ejaculation. The six
conditions are discussed in order of frequency.
Premature Ejaculation
Time and time again premature
ejaculators of many years’ standing not only lose confidence in their
own sexual performance but also,
unable to respond positively while questioning their own masculinity,
terminate their sexual
functioning with secondary impotence. This stage of functional involution is,
of
course, the crowning blow to
husband and wife as individuals and usually to the marital relationship.
Masters &
Johnson, 19701
The Problem
A couple in their late 20s and married for
three years was concerned about the
man’s ejaculation. For religious reasons,
they had not attempted intercourse before
marriage. Since they were married, he
regularly ejaculated before attempts at vaginal
entry. As a result, their union had not
been “consummated.” Her sexual desire
diminished considerably over the three
years of their marriage. Apart from embarrassment
and diminished sexual pleasure that they
both experienced, they wanted
to have children and for her to become
pregnant in the “natural way.” Ejaculating
quickly was not a new problem for him.
Since the first time he attempted intercourse
at the age of 14, he was unable to
accomplish vaginal entry except on one
occasion, and, then, he ejaculated in a
matter of seconds. Since the “squeeze technique”
described by Masters & Johnson1
was tried and found not helpful, the couple
felt desperate and anticipated separation
and divorce if another way to help them
could not be found.
A couple in their mid-50s and married for
25 years was seen because of erectile and
ejaculation problems. Sexual difficulties
began about five years before and were
gradually becoming worse. The husband was
aware of the association between
sexual dysfunctions and diabetes (a disease
with which he lived in the previous 20
years) but until recently had not
volunteered information to his physician about his
sexual difficulties. He believed that the
onset of his (generalized) erectile problems
preceded his ejaculation difficulty by
about one year. He described ejaculating rapidly
after a frantic process of gaining vaginal
entry and before any softening of his
erection made continued containment
impossible.
Terminology
Patients often use the word
“come” to describe an ejaculation/orgasm and “Premature
Ejaculation” when this process
happens too quickly. When the term, Premature Ejaculation
(PE), is used by health
professionals, some consider it to be pejorative and value
laden. Preferring a more
descriptive term, McCarthy has suggested Early Ejaculation as
an alternative2
(p. 144). Others have also used the term, Rapid Ejaculation.3,4
These
terms indicate that speed of
ejaculation is on a continuum from slow to fast rather
than a normal/abnormal dichotomy.
For reasons of consistency with DSM-IV5 and
DSM-IV-PC6 nomenclature,
as well as the inclusion of the concept of control in the
definition (see immediately
below), the term, Premature Ejaculation, will be used in this
chapter.
Definition
Definition problems abound in
attempts to clarify PE. Does one use a time element?
(Critics say that no one carries
a stopwatch to bed.) Or is it better to specify the number
of movements or thrusts? (One
might legitimately ask: just what is the “correct”
number?) Should one follow the
Masters and Johnson suggestion that the woman be
“satisfied” 50% of the time when
intercourse occurs?1 (p. 92) (On the
presumption that
“satisfaction” means “orgasm,” of
what relevance is the Masters and Johnson definition
to a man who is having
intercourse with a woman who comes to orgasm only with
direct clitoral stimulation and
not with intercourse?)
Usually no one debates the issue
of the definition of prematurity when a heterosexual
man ejaculates before, during, or
immediately after vaginal entry. Definition
problems arise with lengthening
of the amount of time after penetration. It is
conceivable that two syndromes
exist: (1) ejaculation before, during, or immediately
after vaginal entry and (2)
ejaculation after vaginal entry but with little or
no control over the timing. It
may be that the former has “premature ejaculation”
and the latter is simply quite
fast and would be reasonably described as having
“rapid ejaculation.”
Grenier and Byers suggest a different
way of considering the definition of PE: there
should be two criteria for the
diagnosis. One is based on the extent of voluntary control
experienced by the man and the
other is based on “latency,” or the amount of time
from vaginal entry to ejaculation.3
Does PE apply to men who are
sexually active with other men? The literature is
unclear on this subject. Masters
and Johnson found that PE “rarely represents a serious
problem to interacting male
homosexuals . . . [since] . . . neither man is dependent
upon the other’s ejaculatory
control to achieve sexual satisfaction”7 (p.
239). However,
another study declared that 19%
of a convenience sample of 197 gay men reported
“ejaculating too soon/too
quickly.”8
If the definition of PE includes
only the speed of ejaculation, the definition
doubtless applies to men sexually
active with other men. However, if the definition
also includes control, the answer
is not so clear. It might depend on the kind of
sexual practices between the two
men. For example, some men might ejaculate rapidly
and out of control during anal
intercourse but rapidly and in control with
mutual masturbation.
Classification
DSM-IV-PC summarizes the criteria
for the diagnosis of PE as follows: “Persistent or
recurrent ejaculation with
minimal stimulation before, on, or shortly after penetration
and before the person wishes it,
causing marked distress or interpersonal difficulty.”6
(This statement introduces a
subjective element by using the phrase “wishes it”). The
clinician is further instructed
to “ . . . take into account factors that affect the duration
of the sexual excitement phase,
such as age, novelty of the sexual partner or situation,
and frequency of sexual
activity.” As with other sexual dysfunctions, clinicians are also
asked to specify if the problem
is lifelong or acquired, or situational or generalized.
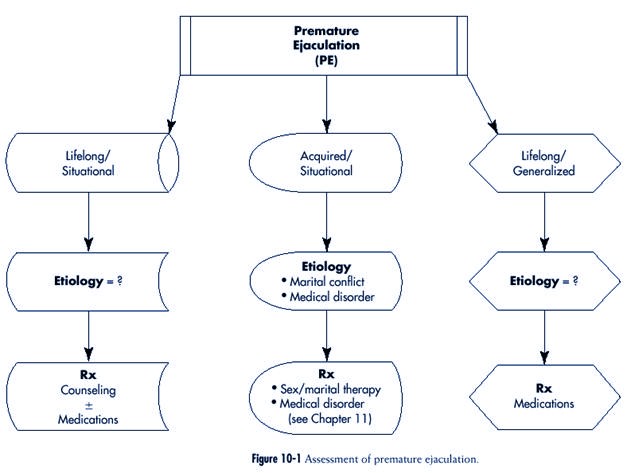
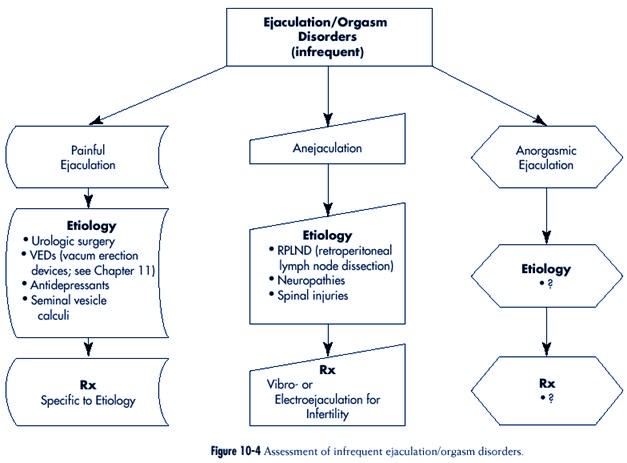
The assessment of premature
ejaculation is outlined in Figure 10-1
Description
The majority of men who ask for
assistance describe a lifelong pattern of ejaculating
quickly and without any control
in attempts at intercourse. This process usually contrasts
with ejaculation with
masturbation, the timing of which is described as entirely
in their control.
History reveals increasing
concern about ejaculation in intercourse after an initial
period in which the man seemed
unaware of possible dissatisfaction of previous sexual
partners (“no one ever said
anything”). His sexual activities tend to focus on intercourse.
On a time scale, the man often
ejaculates within seconds after vaginal entry.
While ejaculation is pleasurable,
the total sexual experience is anything but, since it is
filled with worry and trepidation
about ‘the same thing taking place that occurred the
last time.’ Various attempts at
controlling ejaculation (including distracting oneself by
nonsexual thoughts or
masturbating before a sexual encounter) have been tried and
found wanting. The patient is
apologetic to his partner and privately self-deprecatory.
The current partner is often
angry because her sexual arousal is repeatedly interrupted.
Her interest in sexual activities
may decline. Sometimes a woman in this situation
believes that the man
deliberately chooses not to control the timing of his ejaculation.
Resulting intra- and
interpersonal tensions can be substantial.
Some men describe difficulties
with the timing of ejaculation of relatively recent
onset and after a lengthy period
in which this was not considered to be a problem by
him or his partner(s). The
distinction between this acquired form and its lifelong counterpart
is important from etiological and
therapeutic viewpoints.
Epidemiology
Some information about “normal”
latency was provided by Kinsey and his colleagues
in their survey of men in the
general population9 (pp. 579-581). While they
did not
seem to consider PE to be a
disorder, curiosity about speed of ejaculation
(rather than definition of the
problem) resulted in them asking
about ejaculation latency (that
is, the estimated average time for ejaculation
to occur after vaginal entry).
The time was two minutes for about
three fourths of the men studied.
Laumann and his colleagues asked
those who were surveyed: “during
the last 12 months has there ever
been a period of several months
or more when you came to a climax
too quickly?”10 pp.368-375)
Twenty-nine percent of the men
answered “yes”—the most common
sexual complaint, by far, of the
men surveyed. Positive answers were
greatest in men who were under
the age of 40 and over the age of 54, married and
divorced (compared to those who had
never married), less educated (i.e., received less
than high school education),
black, in poor health, and unhappy.
PE has varied from 15% to 46% of
presenting complaints at sexual problem clinics
in a review of studies completed
between 1970 and 1988.11 Furthermore,
for unknown
reasons, PE may be decreasing
over time as the principal sexual concern of men who
appear at the clinics.
Question: “During the last 12 months
has there ever been a period of several
months or more when you came to a
climax too quickly?” Twenty-nine percent
of the men surveyed answered,
“Yes.” (This is, by far, the most common
sexual complaint of the men surveyed.)
|
The acquired form of PE
(sometimes referred to as “secondary”) is characterized by:
(1) an older man, (2) a briefer
interval of time existing between beginning of the difficulty
and seeking professional
assistance, and (3) erectile difficulties preceding the
onset.12
Etiology
The variety of psychologically
and biologically based etiological hypotheses for PE
have been thoroughly reviewed3
and include the following:
1. Psychodynamic theories
(excessive narcissism or a virulent dislike of women)
2. Early experience (conditioning
based on haste and nervousness)
3. Anxiety (causing activation of
the sympathetic nervous system or distraction
from worry resulting in lack of
awareness of sensations premonitory to ejaculation)
4. Low frequency of sexual
activity
5. Not using techniques that
other men have learned to control the timing of ejaculation
6. Not considering rapidity of
ejaculation to be a disorder, since it is a superior trait
from an evolutionary viewpoint
7. Easier arousal
8. Greater sensitivity to penile
stimulation
9. Malfunctioning of the normal
ejaculatory reflex3
Theories about PE represent
etiological speculations concerning men
who are otherwise healthy.
However, PE has also been reported in
association with trauma to the
sympathetic nervous system during surgery
for aortic aneurysm, pelvic
fracture, prostatitis, urethritis4 and
neurological diseases such as
multiple sclerosis2 (p. 148).
While the presence of anxiety
often seems to be associated with PE,
the direction of the relationship
(cause or effect) is unclear. What is
striking, however, is the fact
that many men (perhaps most) who ejaculate unpredictably
with a partner are able to
control the timing of their ejaculation when masturbating.
(A few men who appear to be
otherwise healthy ejaculate spontaneously and
without control in the presence
of any kind of sexual stimulation.)
Assuming a relationship between
anxiety and ejaculatory control, anxiety
is helpful as an explanation for
the occurrence of PE only in relation
to intercourse (since men are
considerably less anxious when masturbating13).
One of the more compelling
hypotheses for PE is that it “may be,
at least in part, the result of a
physiologically determined hypersensitivity
to sexual stimulation,” that is,
PE may be a reflection of a
lower ejaculatory threshold. In a
study that adds support to this
idea, speed of ejaculation was compared
in premature and nonpremature
ejaculating men when
masturbating. Assessment of latency to ejaculation
showed that when at home the men
with PE ejaculated in about half the time as
their counterparts (three minutes
versus six minutes).11 The authors of this study
suggest a diathesis-stress model
in which “some individuals with a particularly strong
Many men (perhaps most) who ejaculate
unpredictably with a partner are
able to control the timing of their
ejaculation
when masturbating.
Speed of ejaculation was compared in
premature and nonpremature ejaculating
men when masturbating. Assessment
of latency to ejaculation showed that
when at home the men with PE ejaculated
in about half the time as their
conterparts (three minutes versus six
minutes).
|
somatic vulnerability may require
little, if any, anxiety in order to manifest their low
orgastic threshold.”
Investigation into the etiology
of the acquired form of PE suggests separation into
two groups: (1) one in which the
patients had a “demonstrable organic cause” (e.g.,
erectile dysfunction as a result
of diabetes) and (2) one in which the men were involved
in disturbed relationships.12
Investigation
History
The history is the key to the
diagnosis of PE in a man who is otherwise healthy. While
history can be obtained from the
man alone, the effect of this syndrome on both sexual
partners is best gauged by
talking directly with each. Issues to inquire about and suggested
descriptive questions (asked of
heterosexual men, although easily adapted to
gay men as well) include:
1. Duration of ejaculatory
difficulty (see Chapter 4, “lifelong versus acquired”)
Suggested Question: Has
ejaculating quickly always been a problem
for you or was there a period of
time when this did not
occur?”
2. Subjective feeling before
ejaculation (see Chapter 4, “generalized versus situational”)
Suggested Question: “If you
compare your ejaculation when having
intercourse to masturbating, how
much warning do you
have that ejaculation is about to
occur in each situation?”
3. Timing of ejaculation (see
Chapter 4, “description”)
Suggested Question: “Do you
ejaculate before, during, or after
vaginal entry?”
4. Speed of ejaculation (see
Chapter 4, “description”)
Question if Answer is “After”: “On
the basis of time, how long does it
take you to ejaculate after
entry?”
Additional Question: “On the
basis of numbers of movements or
thrusts, how many occur before
you ejaculate?”
5. Methods used to control
ejaculation (see Chapter 4, “description”)
Suggested Question: “Have you
tried to control the timing of
your ejaculation?”
If the Answer is “Yes,” Follow-up
Suggested Question: “What methods have
you used to do this?”
Additional Question: “For
Example, Many Men Stop Moving (or use
condoms, anesthetic creams or
oils, or think of something
nonsexual) in an Attempt to
Prevent Themselves From Getting
Close. Is That Something You’ve
Tried to Do?”
6. Subjective feeling of orgasm
(see Chapter 4, “description”)
Suggested Question: “Although
orgasm is difficult to describe,
can you explain what it feels
like when you ejaculate?”
Additional Possible Question: “Is
it a pleasant or unpleasant experience
for you?”
7. Description of emission (see
Chapter 4, “description”)
Suggested Question: “Men
usually experience repeated or rhythmic
contractions when they ejaculate
so that the semen comes
out in spurts. Do you notice
these contractions when you
ejaculate?”
Additional Suggested Question: “When
ejaculation occurs, does the
semen come out in spurts or does
it dribble out?”
(Comment: There is less force to
ejaculation when there is some obstruction [e.g.,
prostatic hypertrophy or urethral
stricture] neurological disorder, and in the aging
process14 [pp.
257-259].)
8. Psychological accompaniment
(see Chapter 4, “patient and partner’s reaction to
problem”)
Suggested Question: “When you
have trouble with ejaculation,
what’s going through your mind?”
Additional Question: “What
does your wife (partner) think?”
Physical and laboratory examinations
In otherwise healthy men, these
investigations add little useful information.
Treatment
Given the substantial frequency
of lifelong Premature Ejaculation in
the community, the focus on
history-taking as the principal diagnostic
technique, the etiological
concentration on the present rather than the
past, and the usefulness of some
brief approaches, treatment of this
disorder is well within the
purview of primary care.
Masters and Johnson described a
talk-oriented treatment method for PE that provides
an “overall failure rate” of 2.7%1
(pp. 92-115 and 367). Perhaps as a result of the
reported benefits, little else
was suggested therapeutically for some time after. Others
also reported positive effects
after treatment but when long-term follow-up studies
Given the prevalence of lifelong Premature
Ejaculation, the focus on historytaking
as the principal diagnostic technique,
the etiological concentration on
the present rather than the past, and
the usefulness of some brief approaches,
treatment of this disorder is well within
the purview of primary care.
|
were done considerably less
robust results were found. A three-year follow-up study
(for example) reported dramatic
changes at the end of treatment for PE in the duration
of intercourse. However,
pretreatment levels returned after three years.15 (Interestingly,
significant improvements in the
duration of foreplay reported at the end of treatment
were found in this study to have
persisted at follow-up.)
Counseling and medications are
presently the mainstays of treatment for lifelong
PE. Obviously, drug prescription
is available only to physicians. However, cooperative
relationships between all
professionals in the health care system increasingly reflect
changes toward improvement in the
quality of patient care.
Pharmacotherapy
Evidence for the utility of drug treatment
of PE is increasing. In case reports and single
blind studies, psychotropic drugs
are noted to interfere with ejaculation as a side
effect.16 Some
investigators reason that this observation could be turned to advantage,
suggesting that a side effect is
not necessarily an adverse effect. The antidepressants
paroxetine,17
sertraline,18 and
clomipramine4 have undergone double-blind testing for
their usefulness in the treatment
of PE (often in smaller doses than that used in the
treatment of depression).
(Paroxetine [Paxil] and sertraline [Zoloft] are selective serotonin
reuptake inhibitors [SSRIs], and
clomipramine [Anafranil] is a chemical hybrid of
a tricyclic and SSRI).
Waldinger and his colleagues
conducted a double-blind, randomized, placebo-controlled
study of paroxetine (40 mg/day
for five of the six weeks of the study [higher
than what is usually prescribed
in treating depression]) in the treatment of PE in 17
men.17 Patients
and partners were questioned separately. The improvement was
described as dramatic and began
in the first days of treatment (suggesting that the
effect was not a result of
diminished psychopathology). No anticholinergic side effects
(a possible problem with
clomipramine, depending on the dose) or effect on erection
function was reported.
Mendels and his colleagues
randomly assigned 52 heterosexual males to an eight
week study of either sertraline
or a placebo administered in a double-blind fashion.18
The drug was given daily and the
dose varied from 50 to 200 mg, depending on the
beneficial response and adverse
experiences of the patient. Sertraline was judged to be
significantly better than placebo
in (1) prolongation of time to ejaculation and (2)
number of successful attempts at
intercourse.
Althof and his colleagues
completed a double-blind placebo-controlled crossover
trial of clomipramine in a group
of 15 otherwise healthy men with lifelong PE who
were also married or cohabiting
with a woman for at least six months.4 Partners
participated
in the study. Results of the
study are as follows:
1. Mean ejaculatory latency
increased almost threefold at a dose of 25 mg/day and
over five-fold at the other
studied dose of 50 mg/day
2. Both partners reported
statistically significant greater levels of sexual satisfaction
3. Some of the women who reported
never previously experiencing orgasm with
intercourse became coitally
orgasmic
4. Over half of the 10 women who
previously reported orgasm during intercourse
indicated that it now happened
more frequently
5. The men reported greater
emotional and relationship satisfaction
However, when the drug was
discontinued, sexual function returned to the level that
existed before the study.
The use of clomipramine on an “as
needed” basis was examined19 in
another study.
Using a double-blind,
placebo-controlled, crossover design, eight men with PE, six
men with PE and erectile
dysfunction, and eight control men were studied. Partners
did not participate in the study.
Subjects took 26 mg of clomipramine or placebo 12
to 24 hours before anticipated
sexual activity. In contrast to the marked beneficial
effect in the men with “primary”
(i.e., lifelong) PE, the authors report that the drug was
not useful in men who had PE and
erectile dysfunction. This result affirms the importance
of subclassification.
A 28-year-old man and his 32-year-old wife
were seen because of his difficulty with
regular ejaculation before vaginal entry.
This pattern of ejaculation had existed
since the beginning of his attempts at
intercourse as a teenager. His wife was
becoming sexually disinterested and
questioned her commitment to the relationship,
particularly because “the biological clock
was ticking” and she wanted to
begin a family. The couple had undergone a
Masters and Johnson-type of treatment
program about one year earlier and found
that the initial gains were shortlived.
1 A one-visit assessment
was conducted with them together, and clomipramine
was prescribed. The couple was seen again
two weeks later, when substantial
improvement was reported in the following:
• His ejaculation latency
• Their sexual relationship
• Other aspects of their life as a couple
Much to the wife’s pleasure, she became
pregnant within two months of the first
visit. The man was seen for a third time
alone because the wife was unable to
accompany him for the visit. He reported
continued improvement in sexual and
nonsexual areas of their life. Telephone
contact was periodically maintained for the
purpose of medication refills.
In a review of pharmacologic
studies into the treatment of PE, Althof asks the following
serious questions.4
1. Should drugs be the first line
of treatment?
2. How should drugs be used?
(daily? the day of intercourse? a duration of weeks?
months? lifetime?)
3. What are the indications and
contraindications? (Used only in the lifelong form?
The acquired form? Prescribed
only for men who do not ejaculate before, during,
or immediately after entry but
want to “last longer?”)
4. What should be the
relationship between drug treatment and psychotherapy?
Althof concludes that all of
these questions require empirical research and are therefore
difficult to answer at the
present time. Some of these questions are considered
below, and the information given
is based more on clinical judgment and experience
than research data.
Should drugs be the first line of
treatment? Drugs may well be used immediately, as follows:
• A man who persistently
ejaculates in an uncontrolled manner with any
form of sexual stimulation and
particularly before vaginal entry
• A couple when talk-oriented
treatment methods are not helpful
• Many single men without
partners
• When talking to a couple is
unproductive even if a couple relationship
exists (e.g., in the case of a
couple raised in a culture where gender roles
dictate that the woman is subservient
to the man and both subscribe to
this philosophy—a situation that
is functionally the same as talking
with the man by himself)
How should drugs be used? Daily
and ad hoc (e.g., clomipramine four hours before intercourse
is expected to occur) administration
methods have been found helpful.
What are the contraindications? There
are two reasons why drug treatment should not
be used in men who have the
acquired form of PE based on relationship discord. First,
PE in this situation is clearly
symptomatic and it makes little sense to treat the symptom
and not the “disease” (i.e., the
relationship discord). Second, the
problem of PE may well be
reversed with attention given to the disrupted
relationship. Furthermore, in
acquired PE associated with erectile
problems, clomipramine treatment
has been shown to be ineffective.
17 On the subject of
contraindications, Althof also counseled that
considerable caution be exercised
in response to requests from men
who want “boundless intercourse
or designer orgasmic capabilities.”4
What should be the relationship
between drug therapy and psychotherapy?
Althof states that there should
not be an either/or attitude to the use of
these treatment methods and that
both may be desirable or necessary.4
“The two treatment approaches are
not to be compared solely in terms
of economics or ejaculatory
latency. Psychotherapy educates, clarifies,
and often addresses other issues
not perceived when the diagnosis was
originally made.” Indeed, if the
physician’s approach to medications is such that psychotherapy
is not used in
conjunction, then, by experience so far, the man is implicitly
being told that he must take this
medication for, perhaps, a lifetime. The implications
of such a treatment decision are
substantial, especially given that many of the men
presenting with the lifelong and
situational form of PE are young and in the early
stages of their sexual
experience.
Counseling
The talking part of the treatment
of someone with PE includes at least four components:
If the physician’s approach to medications
is such that psychotherapy is not
used in conjunction, the man patient is
implicitly being told that he must take
this medication for (perhaps) a lifetime.
The implications of such a treatment
decision are substantial, especially since
many men presenting with the lifelong
and situational form of PE are young
and in the early stages of their sexual
experience.
|
• Information
• Specific techniques
• Adaptation
• Attention to psychological
issues
Some are easily incorporated into
primary care practice.
INFORMATION
PE-related self-help books seem
to be particularly useful in providing two elements
of counseling20-22:
• Information (in this instance
about men and sexual issues)
• Specific advice (in this
example about controlling ejaculation)
The extent to which these two
elements are therapeutically helpful is unclear, since
men who benefit greatly from such
books would not be likely to seek assistance from
health professionals. Judging by
the reaction of patients to whom such books are suggested,
many find the content to be at
least informative and reassuring and some follow
the specific treatment methods
suggested. Apart from specific issues around ejaculation
control, Zilbergeld, in
particular, interests male readers when discussing the
powerful and influential sexual
“myths” that so often determine how men think and
behave sexually—in their own eyes
and in those of their sexual partners.20,22 This
is
“sex education” as it should be,
that is, the description of body parts and their function
and the discussion of sex-related
aspects of human relationships. Kaplan’s book includes
information about PE and specific
techniques for ejaculatory control (see immediately
below).21
SPECIFIC TECHNIQUES
A second element in counseling,
more applicable to couples, is directed at specific
techniques to control the speed
of ejaculation. Two approaches were described in the
past: “stop-start”23
and the “squeeze technique”1 (pp.
102-104). The stop-start technique
is more popular among sex
therapists because it is easier for health professionals
to explain and for patients to
use. The stop-start approach involves an exercise in
“communication” and comprises at
least four steps:
1. Both partners initially agree
not to attempt intercourse on at least several occasions
(this is essential)
2. The woman stimulates the man’s
erect penis until he is close to ejaculation at
which point he signals her to
stop
3. This happens three or four
times on any one sexual occasion before he eventually
ejaculates
4. The couple then integrates
this into intercourse experiences with frequent
“pauses”
ADAPTATION
An additional facet of
counseling, also more directed to couples, is incorporated
into the concept of adaptation.
Even if little change develops in the timing or speed of
ejaculation as a result of
talking forms of treatment, a considerable shift may occur in
the sexual experiences of the
couple such that the timing of the man’s ejaculation
becomes a lesser or even
nonissue. For example, if the usual “order” of sexual events is
such that the man ejaculates
before his partner is stimulated, this process can be altered
so that attention is given to the
woman’s satisfaction and (possibly) orgasm, before or
after vaginal entry occurs. The
notion of adaptation is consistent with some results
found at follow-up, namely that
treatment of PE may change aspects of foreplay rather
than ejaculatory control.12
PSYCHOLOGICAL ISSUES
Ignoring concurrent psychological
issues in the counseling process decreases the
potential for a good outcome.
A couple in their late 30s, married for 15
years, was referred because the man
regularly ejaculated immediately after
vaginal entry, a pattern that existed throughout
all of his life. In the process of
initially talking with both (together and separately)
it became clear that she was angry and “at
the end of (her) rope.” She was
seriously considering separation for sexual
and nonsexual reasons. Sexually, her
level of interest was similar to her
husband’s (i.e., substantial) but her sexual arousal
was interrupted continually by his
ejaculation. She was orgasmic with direct clitoral
stimulation before intercourse but this was
irregular and unpredictable. Her
animosity toward her husband about
nonsexual concerns related to his inclination
to continually avoid talking about
contentious issues (including their sexual troubles).
It was evident that simply delaying his
ejaculation by using pharmacotherapy
would not circumvent the discord between
the two. Thus deliberate decision was
made to treat this couple using traditional
counseling methods.
Psychological issues may be
particularly important in the solo male. A man might ask
for solo treatment for several
reasons:
1. He may not have a partner
2. Confidentiality and trust
issues may prevent the involvement of a new partner
3. A partner may be unwilling or
unable to participate in the process (this is less
frequent than many men report)
In such circumstances, it is
usually best to explain that although much can be accomplished
diagnostically in seeing him
alone, the absence of a sexual partner is often
therapeutically limiting. Some
aspects of the multifaceted treatment approach described
above can be applied to the solo
male, including the provision of information and
learning specific techniques such
as stop-start while masturbating.
When the limitations of solo
(versus couple) treatment are discussed, clinicians frequently
meet with a “catch-22” response
in which the man says that the very existence
of this problem prevents
establishment of a relationship. He is, in effect, saying that
speed of ejaculation is a
determining force in relationships between men and women—
a suggestion that (to say the
least) not everyone supports. The fact that a partner is not
present to possibly refute this
argument puts the health professional in the difficult
position of presenting a
different point of view to the patient and potentially disrupting
the professional relationship in
the process. Psychotherapy might be helpful to the
extent that the man is prepared
to examine all aspects of a failed relationship, sexual
and otherwise.
Indications for Referral for Consultation or Continuing
Care by a Specialist
1. Consultation with a physician
is required when pharmacotherapy is considered
and the health professional is
trained in a different discipline.
2. In the acquired form of PE
associated with relationship discord, the ejaculation
issue is likely symptomatic and
treatment would involve relationship therapy—
a process that is best undertaken
on a continuing care basis by those in the
health care system with clinical
experience in this area, that is, mental health
professionals.
3. In the acquired form of PE
associated with an erectile disorder, managing both
problems may be complex. Therefore
referral to a sex-specialist for continuing
care may be necessary.
4. Care of the solo man, beyond
the use of drugs, often presents a dilemma.
Men who are unwilling to use
pharmacotherapy or who continue to have
inter- or intrapersonal
difficulty despite slower ejaculation are best seen for
continuing care by a mental
health professional who is comfortable with sexual
issues.
5. Unsuccessful treatment at the
primary care level should result in referral to a
sex-specialist, at least for consultation,
and possibly for continuing care.
Summary
Premature Ejaculation (PE) in
heterosexual men is difficult to define precisely except
in situations where ejaculation
occurs persistently before, during, or immediately
after vaginal entry. Control over
the process of ejaculation appears to be a significant
element in the definition, as
well as the duration of time between vaginal entry
and ejaculation. Most men with
this disorder describe a lifelong pattern. “Coming
to a climax too quickly” was the most
common sexual complaint registered by
men in a substantial survey of
sexual behavior. An unreplicated study suggests an
appealing hypothesis for the
etiology of the lifelong form of PE, namely, that it is
partly related to a
“physiologically determined hypersensitivity to sexual stimulation.”
The acquired form seems to be the
result of relationship discord or medical
illness. The focus of
investigation into the lifelong form of PE is particularly on
history-taking (rather than
physical examination or laboratory studies). Counseling
and medications are the mainstays
of treatment of this disorder. The latter has
demonstrated great value,
although many details concerning drug treatment have
yet to be elaborated.
Long term follow-up studies of
counseling alone show modest results. The potential
value of combining the two
treatment forms has not been investigated. Intuitively,
medications may be considered a
short-term intervention, and psychotherapy may be
included toward the long-term
goal of permanent change. Referral for consultation
with a physician is required when
drug therapy is undertaken by a health professional
from another discipline. Referral
for continuing care is particularly reasonable in the
acquired form of PE and when
slowing of ejaculation in a man seen alone has resulted
in limited success in allowing
him to develop intimate relationships.
Delayed Ejaculation/Orgasm
Terminology
This syndrome has been variously
called:
• Ejaculatory Incompetence1
• Retarded Ejaculation24
• Male Orgasm Disorder5,6
An evident problem with the terms
is the confusion about whether this is a disorder of
ejaculation, of orgasm, or both.
These two phenomena are separate from a neurophysiological
viewpoint although usually
tightly interwoven. The separateness is evident
in the normal development of
preadolescent boys who are able to come to orgasm
but who cannot ejaculate because
the mechanism is not fully developed. The term,
Delayed Ejaculation/Orgasm (DE/O),
is preferred because it is entirely descriptive and
DE/O refers to a delay in both
ejaculation and orgasm.
Definition
Defining DE/O presents problems
similar to PE, namely, the question of how much
time constitutes a delay? In one
form, the definition of time is not a problem, since
the man can ejaculate without
difficulty when alone (without any delay), but usually
not at all when with a partner.
When ejaculation is truly delayed, it is slow in all
situations—regardless of the
sexual activity and the nature of the partnership. In fact,
ejaculation/orgasm may be so
delayed that the person stops trying. In either case
(delayed or absent) the
definition is usually provided by the patient as he, for example,
compares his present experience
to that of the past or receives complaints from
a sexual partner who may become
vaginally uncomfortable because of a lengthy
period of intercourse.
Classification
In DSM-IV-PC, orgasm difficulties
for men and women are classified similarly6 (p.
117). “Male Orgasmic Disorder” is
defined as: persistent or recurrent delay in, or
absence of, orgasm after a normal
sexual excitement phase. This can be present in all
situations, or present only in
specific settings, and causes marked distress or interpersonal
difficulty. Additional clinical
information is provided: “In diagnosing Orgasmic
Disorder, the clinician should
also take into account the person’s age and sexual experience.
. . . In the most common form of Male Orgasmic Disorder, a male cannot
reach orgasm during intercourse,
although he can ejaculate with a partner’s manual or
oral stimulation. Some males. . .
. can reach coital orgasm but only after very prolonged
and intense noncoital
stimulation. Some can ejaculate only from masturbation.
When a man has hidden his lack of
coital orgasm from his sexual partner, the
couple may present with
infertility of unknown cause.” Determining the subclassification
as lifelong or acquired,
generalized or situational can be crucial to determining
etiology and treatment.
The assessment of Delayed
Ejaculation/Orgasm is outlined in Figure 10-2.
Description
DE/O presents clinically in one
of two forms:
• Situational
• Generalized
When situational, the problem is
usually lifelong rather than acquired. When generalized,
it is much more likely to be
acquired.
In the situational form, the
history is usually one of ejaculation without difficulty
when alone but inability to
ejaculate with partners generally or during a specific sexual
activity, typically intercourse.
The request for assistance often can be traced to the
partner and characteristically
results from vaginal discomfort, concerns about reproduction,
or both. Sometimes the man
describes a method of masturbation that is difficult
to transfer to sexual activity
with a partner (e.g., rubbing his penis against a firm
surface rather than using his
hand).
Two gay men in their 20s were seen because
one was unable to ejaculate in the
presence of the other while having no such
difficulty when masturbating alone.
Strains in their relationship became
apparent when the sexually functional partner
let it be known that he considered his
partner’s inability to ejaculate to be a form
of rejection. History revealed that the man
with DE/O experienced this pattern of
ejaculation in previous brief sexual
relationships as well as the three he considered
long-term. Treatment using the approach
described by Masters and Johnson was
unsuccessful at reversing the pattern1
(pp. 129-133). One-year follow-up revealed
that the relationship had dissolved.
In the generalized form (lifelong
or acquired), history reveals that the man is experiencing
substantial delay or absence of
ejaculation/orgasm in all circumstances. Typically,
the history is brief and clearly
indicates that this is acquired and dates from the
onset of the use of a particular
medication (see “Etiology” below in this chapter). Occasionally
this may be life long. Cultural
or religious beliefs may also be a critical factor.
On some occasions, the history
reveals a hybrid form, that is, one that has characteristics
of both syndromes. Ejaculation is
possible but only during masturbation.
When ejaculation does occur in
such circumstances, vigorous and lengthy penile
stimulation is usually
required—much more so than can be provided by vaginal
intercourse.
A 35-year-old single man described an inability
to ejaculate with a partner in spite
of intercourse lasting up to one hour.
Women partners initially enjoyed the experience
and would find themselves repeatedly
orgasmic. However, this attitude
was soon replaced by one of impatience as
the pleasure was superseded
by the vaginal discomfort accompanying the
long duration of
intercourse. He described being able to
ejaculate only with masturbation
in a process that required about 15 minutes
and great physical exertion
in which he “worked” so hard he would
sweat. He forcefully rubbed
his penis against a hard surface while
fantasizing about himself dressed
as a woman.
In the Lauman study,10
8% of men
reported being “unable to orgasm.”
(The investigators did not apparently
distinguish between ejaculation/orgasm
that was delayed and that which was
entirely absent.)
|
Epidemiology
In the Laumann study, 8% of men
reported being “unable to orgasm”10(pp.
370-374).
(The investigators did not
apparently distinguish between ejaculation/orgasm that was
delayed and that which was
entirely absent.) The age category in which this syndrome
was reported with greatest
frequency was the 50 to 54 year old group (14%). Inability
to come to orgasm was also
reported more commonly in “Asian/Pacific Islander” men
(19%), as well as those who were
poorly educated (13%—less than high school), and
financially poor (16%). As with
other dysfunctions, the percentages of affected men
increased with diminished health
(18% of those whose health was “fair”) and happiness
(23% of men who were “unhappy
most times”).
“Male Orgasm Disorder” accounted
for 3% to 8% of cases presenting for treatment
in a review of clinical studies.11
Etiology
In the situational and hybrid
forms, it is evident that specific sexual and/or psychosocial
factors are central to
etiological speculations25 (pp.179-185);
1(p. 126). Theories
include:
1. That some men are highly
reactive genitally
2. That some men are fearful of
dangers associated with ejaculation
3. An inhibition reflex
4. Religious orthodoxy
5. Male fear of pregnancy
6. Sexual interest in other men
7. A psychologically traumatic
event
In the acquired and generalized
form, there is often a history of recent
use of a medication that is known
to interfere with ejaculation/orgasm (see Appendix
V) or the presence of a
neurological disorder such as multiple sclerosis.
“All of the drugs approved for
the treatment of depression or the treatment of
obsessive-compulsive disorder in
the United States, with the exception of nefazodone
and bupropion, have been reported
to be associated with ejaculatory or
orgasmic difficulty.”26
Prevalence figures for any one of the drugs varies as a result
of different sources
(manufacturer or published report) or variations in methodology
(spontaneous reports or direct
inquiry). Ejaculatory problems (delay or inhibition)
have been reported in patients
taking the following drugs:
• Imipramine (30%)
• Phenelzine (40%)
• Clomipramine (96%)
• Fluoxetine (24% to 75%)
• Sertraline (16%)
• Paroxetine (13%)
• Venlafaxine (12%)
Some antihypertensive drugs also
interfere with ejaculation/orgasm. One of the problems
in investigating the extent of
this problem is that hypertension can cause sexual
All drugs approved for treatment of
depression or obsessive-compulsive disorder
in the United States with the
exception of nefazodone and bupropion
are reported to be associated wih
ejaculatory
or orgasmic difficulty.26
|
difficulties apart from the drugs
used in its treatment. “Ejaculatory dysfunction” was not
found at all in two studies that
included normotensives, but was associated with 7% to
17% of untreated, and 26% to 30%
of treated patients27 (p. 204). Antihypertensive
drugs that can cause sexual
difficulties were reviewed27: and, in
relation to delayed
ejaculation, specifically included
the following:
• Reserpine (p. 216)
• Methyldopa (p. 219)
• Guanethidine (p. 224)
• Alpha1 blockers
(p. 235)
• Alpha2 agonists
(p. 237)
• Calcium channel blockers (p.
245)
Notably missing from this list
were the following:
• Diuretics (p. 210)
• Beta-blockers (p. 227)
• ACE inhibitors (p. 242)
Investigation
History
1. Duration (see Chapter 4,
“lifelong versus acquired”)
Suggested Question: “Has
ejaculation difficulty been a problem all
your life or is it a problem that
developed recently?”
2. Ejaculation with a partner
(see Chapter 4, “generalized versus situational”)
Suggested Question: “Do you
ejaculate at all now when you are
with a partner?”
Additional Question if the Answer
is “No”: “Have you ever ejaculated with
a partner?”
Additional Question if the Answer
to Either Previous Question is “Yes”: “What kind
of sexual activity resulted in
your ejaculation (e.g., intercourse
or oral stimulation)?”
3. Ejaculation with masturbation
(see Chapter 4, “generalized versus situational”)
Suggested Question: “Do you
ejaculate now when you masturbate?”
Additional Question if the Answer
is “No”: “Have you ever ejaculated
when you masturbated?”
4. Feeling prior to
ejaculation/orgasm (see Chapter 4, “description”)
Suggested Question: “Do you
sometimes feel that you are close to
ejaculation/ orgasm but then the
feeling disappears?”
Additional Question: “When
with a partner, Do you ever pretend
that you have come to orgasm?”
Physical and Laboratory Examinations
In an otherwise healthy man, no
particular physical or laboratory examinations are
required.
Treatment
In the care of men with the
situational form of DE/O, reported series are few. Masters
and Johnson described their
treatment format and their five-year follow-up of 17 men
and reported a treatment failure
rate of 17.6%1 (pp. 116-136, p.357). Another threeyear
follow-up study in the United
States described the treatment of five men15 who
reported themselves as:
Three men Improved
One man The same
One man Worse
A one to six year follow-up study
conducted in the United Kingdom
described two cases of
“ejaculatory failure” and reported that in one
there was no change, and in the
other, the problem was resolved
although still experienced.28
No other case studies involving large
numbers of patients have been
published.
On the basis of impression rather
than data, the occasional man with DE/O asks for
care in his teens, and soon after
intercourse experiences have begun. Such men may be
amenable to the reassurance and
provision of information that often comes with history-
taking alone. The health
professional might be justifiably optimistic about the
result in such circumstances.
Unfortunately, in most instances, men with DE/O do not
ask for treatment until years
later when they are pressured into it by a sexual partner.
By that time, many sexual
experiences have taken place (either alone or with partners)
with a particular method of
ejaculation, a pattern that may have become crystallized
and difficult to change.
In the generalized form of DE/O,
and when there is reason to suspect the use of a
medication in the etiology, the
following treatment “strategies” are suggested:
1. Maintain dosage of the
medication and wait for tolerance to develop
2. Reducing the dosage
3. Change the regimen (e.g., the
use of a “drug holiday”)29
4. Change to an alternative
medication (e.g., when the sexual side effects of sertraline
and nefazodone were compared in
the treatment of depression, nefazodone
was said to have no inhibitory
effects on ejaculation)30
5. Administer a second medication
to counter the sexual side-effect of the first (see
immediately below)26
Men with DE/O usually do not ask for
treatment until they are pressured into
it by a sexual partner. By then, many
sexual experiences may have taken
place, resulting in a firmly established
pattern of ejaculation that may be
difficult
to change.
|
Two potential problems exist when
using other medications at the same time: the clinician
must ensure that the second
medication does not counteract the therapeutic impact
of the first, and sexual
spontaneity inevitably diminishes somewhat when planning
precedes the sexual event
(although often an exaggerated patient concern).
Segraves described seven
medications that have been used in an effort to control
the sexual side-effects of
antidepressants (mostly SSRIs): bethanechol, cyproheptadine,
yohimbine, amantadine, bupropion,
dextroamphetamine, and penoline.26 Methylphenidate
has been suggested31
also, as well as intermittent nefazodone32 (Box
10-1 and
Table 10-1).
Since outcome research has not
subclassified patients, one can only provide clinical
impressions about the generalized
and lifelong form of DE/O. Given that biological
factors likely explain the
etiology, helping the patient adapt through the provision of
information seems the optimal
approach.
Box 10-1
Strategies in Treating Delayed Ejaculation/Orgasm due to Antidepressant Drugs
1. Wait for tolerance to develop
2. Decrease dosage
3. Change regimen (e.g., “drug holiday”)
4. Use alternate drugs
5. Use additional drugs (“antidotes”)
|
 1
1
Indications for Referral for Consultation or Continuing
Care by a Specialist
1. Situational DE/O: If this
pattern of ejaculation has existed for some years, referral
for sex therapy for the purpose
of continuing care may be most beneficial
2. Acquired and generalized DE/O:
where medications seem etiologically significant
but the symptom has not altered
with the strategies outlined in Box 10-1, it
is reasonable to ask for advice
(consultation) from a physician who has expertise
in the use of the particular
class of drugs.
3. Lifelong and generalized DE/O:
if the provision of information and reassurance
about the likely positive outcome
proves insufficient, referral to a sex therapist
for continuing care is the next
logical step
Summary
Delayed Ejaculation usually
represents a disorder (delay or absence) of both ejaculation
and orgasm, hence the use of the
abbreviation, “DE/O.” The disorder appears in
two forms:
• Situational, in that the man
can come to ejaculation/orgasm without
problem when alone but has great
difficulty when a partner is present
• Generalized in the sense that
the man has difficulty under all circumstances
(with a partner or when alone
with masturbation)
While unusual, the problem of
delayed ejaculation is by no means rare (8% of men in
one community survey indicated
inability “to orgasm”). Etiologies are as follows:
1. The situational form includes
significant psychosocial factors
2. The lifelong and generalized
form includes biological factors that have not yet
been defined
3. The acquired and generalized
form can usually be explained by the use of medications
(especially medications used in
Psychiatry and in the control of hypertension)
or the onset of a neurological
disorder
The effects of treatment in the
situational form seem better when the duration of the
problem is brief. Several
approaches are suggested for the generalized and acquired
form where the etiology is
related to medications. Treatment for the lifelong and generalized
form can generally be undertaken
initially on a primary care level through the
provision of information and
reassurance. Men with the acquired and generalized form
who have never ejaculated in the
waking state require care from a specialist.
Retrograde Ejaculation
Definition
Retrograde ejaculation (RE) “is
the propulsion of seminal fluid from the posterior urethra
into the bladder”.33
What is usually referred to as “ejaculation” actually comprises
three separate events34
(p. 423):
• First, “emission”
• Second, closure of the “bladder
neck”
• Third, “ejaculation”
Emission involves the deposition
of seminal fluid from the vas deferens, the seminal
vesicles, and prostate gland into
the posterior urethra. Ejaculation refers to the expulsion
of semen from the penis, which,
in turn, requires simultaneous closure of the
muscular valve at the junction
between the urethra and bladder (the bladder “neck”).
This blockage prevents the semen
from traveling backward into the bladder instead of
going forward out the end of a
man’s penis. The expulsion of semen (true ejaculation)
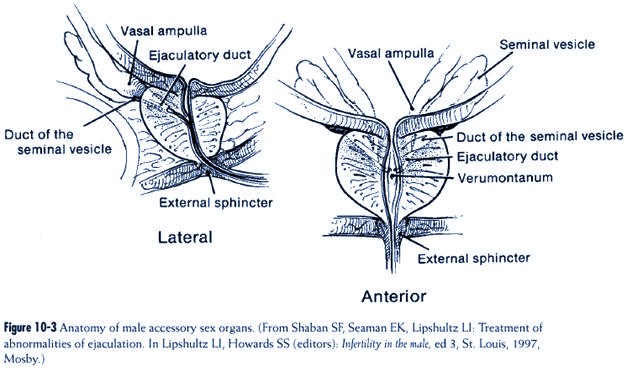
also involves intermittent
relaxation of the “external sphincter”; there are three to seven
contractions about 0.8 seconds
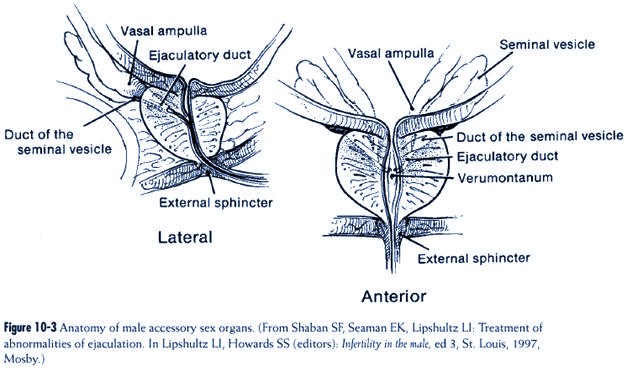
apart (see Figure 10-3).
The final portion of this process
comprises rhythmic contractions of the bulbospongiosus
and ischiocavernosus muscles,
resulting in forward movement of seminal fluid
through the anterior urethra and
emerging from the penile meatus. Orgasm is considered
a cerebral event that occurs
together with emission or ejaculation and associated
with unknown physiological
mechanisms35 (p. 155).
Emission and bladder neck closure
appear to be predominantly under the control of
the sympathetic portion of the
autonomic nervous system, and the expulsion of semen
is predominately under the
influence of the somatic nervous system35 (pp.
165-166).
“Any interference (anatomical,
traumatic, neurogenic or drug-induced) with (the integrity
of these systems) may result in
abnormal function of the internal sphincter of the
urethra, and favor retrograde
ejaculation (RE) as the path of least resistance”.36
Etiology
One way of considering
etiological factors in RE is to separate them into (1) ones that
disrupt the anatomy of the
sphincter at the bladder neck and (2) ones that interfere
with this sphincter’s function37
(p. 383). The best example of an anatomical disruption
of this sphincter is a
transurethral prostatectomy (TURP). Examples of factors that
interfere with function of this
sphincter include the following:
1. Retroperitoneal lymph node
dissection (RPLND) or total lymphadenectomy in
the treatment of some testicular
cancers
2. Diabetes
3. Abdominopelvic surgery
4. Spinal cord injury
Some medications can induce a
pharmacologic “sympathectomy” resulting in failure of
emission and/or bladder neck
closure (see Appendix V). These drugs34 (p. 427)
include
the following antipsychotics
(e.g., chlorpromazine and Haldol), antidepressants (e.g.,
amitriptyline and SSRIs),
antihypertensives (e.g., guanethidine, diuretics and prazosin),
and others (including alcohol).
Epidemiology
RE seems to be common as a
complication of TURP but the actual frequency is not
entirely clear. In one study of
men before and after surgery, 24% who had no presurgical
difficulty with ejaculation
answered “yes” to the following question after surgery:
“Do you have difficulty with
getting the sperm out?”38 However,
37% of the
men who had no presurgical
difficulty also said that they had no ejaculatory problem
afterward.
Given the frequency with which RE
seems to occur as a result of
TURP, the aging of the population
(assuming TURP continues to be
medically popular as a treatment
of benign prostatic hypertrophy)
might well result in an increase
in the prevalence of RE.
RE seems to be infrequent as a
cause of infertility in men (up to
2%)37 (p.
383).
Investigation
History reveals that the patient
reports not ejaculating while (in the
majority of cases) continuing to
experience orgasm (“dry orgasm”). The
definitive diagnosis is made by
laboratory examination of the man’s
urine immediatly after orgasm,
and finding spermatozoa in the sample.
Treatment
Most men who develop RE as a
consequence of TURP accept this situation and do not
ask for treatment. When care is
required (usually because of infertility), RE is best
managed by physicians. The focus
of infertility treatment is on attempting to induce
antegrade ejaculation by
increasing sympathetic tone at the bladder neck or diminishing
parasympathetic activity.33
Alpha-adrenergic agents are commonly used to enhance
Most men who develop RE as a consequence
of TURP accept this situation and
do not ask for treatment. When care is
required (usually because of infertility),
RE is best managed by physicians. The
focus of infertility treatment is on
attempting to induce antegrade ejaculation
by increasing sympathetic tone at
the bladder neck or diminishing
parasympathetic
activity.33
|
sympathetic tone. In a detailed
study of one patient who stopped ejaculating as a result
of lymphadenectomy, four such
drugs were used39 and all seemed equally efficacious:
1. Dextroamphetamine sulphate, 5
mg four times daily
2. Ephedrine, 25 mg four times
daily
3. Phenylpropanolamine, 75 mg
twice daily
4. Pseudoephedrine, 60 mg four
times daily
The study concluded that
long-term treatment was consistently more effective than a
single dose. Elliott (personal
communication, 1997) found that in patients who have
RE as a result of a spinal injury
the effects of pseudoephedrine, in particular, can diminish
if used continuously for more
than four days, and that it may be more useful to use
it on an “as needed” basis
Anticholinergics have also been used successfully (brompheniramine
8 mg twice daily) and imipramine
(25 to 50 mg daily). Surgery has also been
suggested.33
When antegrade ejaculation can not
be restored the treatment of infertility involves
inseminating the woman with sperm
cells taken from the urine by the process of centrifugation.
In one group of eight patients
with RE, the combination of alkalinization
of the urine, immediate removal of
sperm cells from the urine, and the implementation
of artificial insemination
techniques resulted in a “fecundity rate” of 45%40 (p.
440).
When psychological concerns
exist, they often relate to surprise and apprehension
if, for example, a patient who has
undergone a TURP was not forewarned about not
seeing semen when he ejaculates.
Psychological concerns may also be about other
accompanying factors such as the
possible presence of erectile or orgasmic difficulties
and infertility. These other
issues can have powerful repercussions.
Indications for Referral for Consultation or Continuing
Care by a Specialist
As an isolated issue, RE does not
appear to be a cause of further sexual difficulties. To
the extent that sexual concerns
are related to information, primary care treatment is
usually sufficient. Consultation
with a sexual medicine specialist may be useful in
instances when RE is associated
with other sexual difficulties. When infertility concerns
result from RE (generally younger
men of reproductive age who have experienced
retroperitoneal lymph node
dissection or total lymphadenectomy for the treatment of
testicular cancer), continuing
care should be undertaken by an expert physician.
Summary
Retrograde ejaculation (RE) is
usually reported by a man as an orgasm without the
associated emergence of semen
(“dry orgasm”). Semen travels “backward” into the
bladder and the definitive
diagnosis can be made by the finding of spermatozoa in the
urine. The most common cause of
RE is the TURP procedure for benign prostatic
hypertrophy. For most men,
information is the only treatment needed. When fertility
is a concern, medical treatment
focus is on the attempt to enhance sympathetic tone
at the bladder neck by using
alpha-adrenergic agents or diminishing parasympathetic
activity. Specialist care is
required only in those instances where there are associated
sexual difficulties or concerns
about infertility.
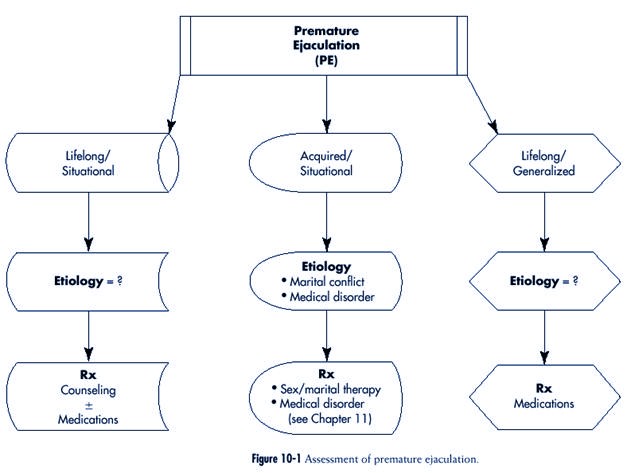
Infrequent Ejaculation/Orgasm Disorders
Infrequent ejaculation/orgasm
disorders include painful ejaculation, anejaculation and
anorgasmic ejaculation. The
assessment of infrequent ejaculation/orgasm disorders is
outlined in Figure 10-4.
Reports of genital pain
associated with ejaculation are uncommon. The following
four causes are known:
1. Some of the tricyclic
antidepressants (amoxapine [related to loxapine], imipramine,
desipramine, clomipramine)41,42
2. Seminal vesicle calculi43
3. Urological surgery
4. Vacuum erection devices (VEDs)
The first two explanations may
not be immediately apparent. When associated with
tricyclic antidepressants,
ejaculatory pain is dose-related so that it diminishes when the
dose is decreased and disappears
when the medication is discontinued.42
The absence of ejaculation, or
anejaculation (antegrade or retrograde), occurs as a
result of peripheral sympathetic
neuropathy44 (pp. 404-6). It occurs in men with spinal
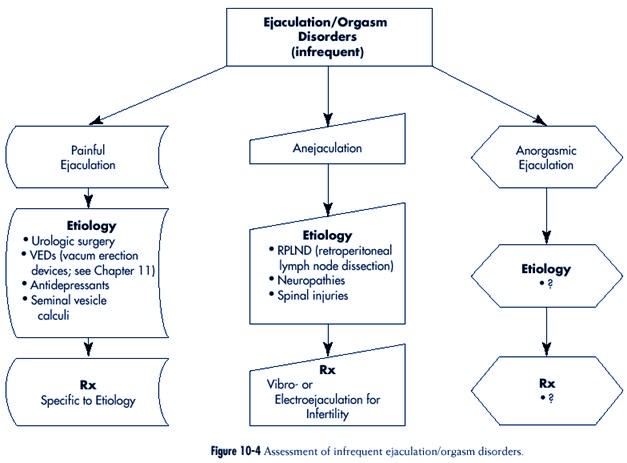
cord injury, men who had
retroperitoneal lymph node dissection (RPLND) for testicular
cancer, and in neuropathies such
as those seen in multiple sclerosis and diabetes.
Diagnosis is based on the absence
of seminal fluid in postejaculatory urine to eliminate
the possibility of RE.
Emission/ejaculation and subsequent pregnancy can result from
the use of specialized procedures
such as vibratory stimulation or electroejaculation.45
Ejaculation without orgasm is
quite unusual judging from the literature and clinical
experience. The etiology is
unknown.
A 47-year-old man was seen with the
complaint of ejaculating without the sensation
of orgasm. He vividly recalled the powerful
feeling of orgasm in the past and
hoped that it would return. The sensation
of orgasm tapered during the past three
years so that it was virtually absent at
the present time—regardless if he ejaculated
with masturbation or with a partner. He had
previously been married for 12 years
and had experienced premature ejaculation
throughout all of the marriage. In four
of the seven years after his divorce, his
sexual experiences with other women were
described with relish, particularly since
he was then free of any ejaculatory difficulty.
His general health was unimpaired, his
sexual desire was as strong as ever,
and he never experienced any erectile
difficulties. When seen one year after his
initial consultation, the problem had not changed.
REFERENCES
1. Masters WH, Johnson VE: Human sexual
inadequacy, Boston, 1970, Little, Brown and
Company.
2. McCarthy BW: Cognitive-behavioral
strategies and techniques in the treatment of early
ejaculation. In Leiblum SR, Rosen RC
(editors): Principles and practice of sex therapy: update for
the 1990s,
ed 2, New York, 1989, The Guilford Press, pp. 141-167.
3. Grenier G, Byers ES: Rapid ejaculation: a
review of conceptual, etiological, and treatment
issues, Arch Sex Behav 24:447-472,
1995.
4. Althof SE: Pharmacologic treatment of
rapid ejaculation. In Levine S (editor): Psychiatr
Clin North Am 18:85-94,
1995.
5. Diagnostic and statistical manual of
mental disorders, ed 4, revised, Washington, 1987, American
Psychiatric Association.
6. Diagnostic and statistical manual of
mental disorders, ed 4, primary care version, Washington, 1995,
American Psychiatric Association.
7. Masters WH, Johnson, VE: Homosexuality
in Perspective, Boston, 1979, Little, Brown
and Co.
8. Simon Rosser BR et al: Sexual difficulties,
concerns, and satisfaction in homosexual men:
an empirical study with implications for HIV
prevention, J Sex Marital Ther
23:61-73,1997.
9. Kinsey AC, Pomeroy WB, Martin CE: Sexual
behavior in the human male, Philadelphia and
London, 1949, W.B. Saunders.
10. Laumann EO et al: The social
organization of sexuality: sexual practices in the United States,
Chicago, 1994, The University of Chicago
Press.
11. Spector IP, Carey MP: Incidence and
prevalence of the sexual dysfunctions, Arch Sex
Behav 19:389-408,
1990.
12. Godpodinoff ML: Premature ejaculation:
clinical subgroups and etiology, J Sex Marital
Ther 15:130-134,
1989.
13. Strassberg DS et al: The role of anxiety
in premature ejaculation: a psychophysiological model,
Arch Sex Behav 19:251-257, 1990.
14. Masters WH, Johnson VE: Human Sexual
Response, Boston, 1966, Little, Brown and Co.
15. De Amicis LA et al: Clinical follow-up of
couples treated for sexual dysfunction, Arch Sex
Behav 14:467-489,
1985.
16. Balon R: Antidepressants in the treatment
of premature ejaculation, J Sex Marital Ther
22:85-96, 1996.
17. Waldinger MD, Hengeveld MW, Zwinderman
AH: Paroxetine treatment of premature
ejaculation: a double-blind, randomized,
placebo-controlled study, Am J Psychiatry
151:1377-1379, 1994.
18. Mendels J, Camera A, Sikes C: Sertraline
treatment for premature ejaculation, J Clin
Psychopharmacology 15:341-346,
1995.
19. Haensel SM et al: Clomipramine and sexual
function in men with premature ejaculation
and controls, J Urol 156:1310-1315,
1996.
20. Zilbergeld B: Male sexuality, New
York, 1978, Bantam Books.
21. Kaplan HS: PE:how to overcome
premature ejaculation, New York, 1989, Brunner/Mazel, Inc.
22. Zilbergeld B: The new male sexuality,
New York, 1992, Bantam Books.
23. Semans JH: Premature ejaculation: a new
approach, South Med J 49:353-358, 1956.
24. Kaplan HS: The new sex therapy: active
treatment of sexual dysfunctions, New York, 1974,
Brunner/Mazel.
25. Apfelbaum B: Retarded ejaculation: a
much-misunderstood syndrome. In Leiblum SR,
Rosen RC (editors): Principles and
practice of sex therapy: update for the 1990s, ed. 2, New York,
1989, The Guilford Press, pp. 168-206.
26. Segraves RT: Antidepressant-induced
orgasm disorder, J Sex Marital Ther 21:192-201,
1995.
27. Crenshaw TL, Goldberg, JP: Sexual
pharmacology: drugs that affect sexual function, New York,
1996, W.W. Norton & Company.
28. Hawton K et al: Long-term outcome of sex
therapy, Behav Res Ther 24:665-675,
1986.
29. Rothschild AJ: Selective serotonin
reuptake inhibitor-induced sexual dysfunction:
efficacy of a drug holiday, Am J
Psychiatry 152:1514-1516, 1995.
30. Feiger A et al: Nefazodone versus
sertraline in outpatients with major depression: focus
on efficacy, tolerability, and effects on
sexual function and satisfaction, J Clin Psychiatry
57(Suppl 2):53-62, 1996.
31. Bartlik BD, Kaplan P, Kaplan HS:
Psychostimulants apparently reverse sexual dysfunction
secondary to selective serotonin reuptake inhibitors,
J Sex Marital Ther 21:264-271, 1995.
32. Reynolds RD: Sertraline-induced
anorgasmia treated with intermittent Nefazodone
(letter), J Clin Psychiatry 58:89,
1997.
33. Hershlag A, Schiff SF, DeCherney, AH:
Retrograde ejaculation, Hum Reprod 6:255-258,
1991.
34. Shaban SF, Seaman EK, Lipshultz LI:
Treatment of abnormalities of ejaculation. In
Lipshultz LI, Howards SS (editors): Infertility
in the male, ed 3, St. Louis, 1997, Mosby, pp.
423-438.
35. Benson GS: Erection, emission, and
ejaculation: physiological mechanisms. In Lipshultz
LI, Howards SS (editors): Infertility in
the male, ed 3, St. Louis, 1997, Mosby-Year Book,
Inc., pp. 155-172.
36. Yavetz H et al: Retrograde ejaculation, Hum
Reprod 93:381-386, 1994.
37. Oates RD: Nonsurgical treatment of
infertility: specific therapy. In Lipshultz LI, Howards
SS (editors): Infertility in the male, ed
2, St. Louis, 1991, Mosby - Year Book, Inc., pp
376-394.
38. Thorpe AC et al: Written consent about
sexual function in men undergoing transurethral
prostatectomy, Br J Urol 74:479-484,
1994.
39. Proctor KG, Howards SS: The effect of
sympathomimetic drugs on postlymphadenectomy
aspermia, J Urol 129:837-838, 1983.
40. Gilbaugh JH: Intrauterine insemination.
In Lipshultz LI, Howard SS (editors): Infertility in
the male, ed
3, St. Louis, 1997, Mosby, pp. 439-449.
41. Kulik FA, Wilbur R: Case report of
painful ejaculation as a side effect of Amoxapine, Am
J Psychiatry 139:234-235,
1982.
42. Aizenberg D et al: Painful ejaculation
associated with antidepressants in four patients, J
Clin Psychiatry 52:461-463,
1991.
43. Corriere JN Jr: Painful ejaculation due
to seminal vesicle calculi, J Urol 157:626, 1997.
44. Hakim LS, Oates AD: Nonsurgical treatment
of male infertility: specific therapy. In
Lipshultz LI, Howards SS (editors): Infertility
in the male, ed 2, St. Louis, 1997, Mosby.
45. Elliott S et al: Vibrostimulation and
electroejaculation: the Vancouver experience, J Soc
Obstet Gyncol Can 15:390-404, 1993.