CHAPTER 9
Low Sexual Desire In Women And Men
While something is known about
how to generate sexual desire—for example, creation of a new intimacy
in a conflicted relationship,
education in how to sexually stimulate one another, and provision of permission
to engage in sensuous
activity—the therapist knows far less than the patient thinks about how to
catalyze the appearance of
(sexual desire) . . . A sexual desire problem begins as a mystery to both
patient and doctor. . .
Levine,
19881
The Problem
A 35-year-old woman described a concern
that from the time of her marriage seven
years ago until the delivery of her 21⁄2
year old child, she became depressed and
irritable the week before her menstrual
periods and also lost all interest in anything
sexual during that time—thoughts, feelings,
or activities. This contrasted with her
“normal” sexual desire at other times,
which she felt were a rich part of her personal
life experience and relationship with her
husband. She was sexually active and
interested during her pregnancy but since
the delivery ceased to be interested in
anything sexual. Her husband was distressed
and she missed the sexual feelings
that had been so important to her in the
past.
A 45-year-old man was seen with his
41-year-old wife. They had been married for
17 years. Eleven years before, she
developed a bipolar illness and had periods of
depression and mania. She was sexually
involved with other men on an indiscriminate
and impulsive basis during her manic
episodes. The couple had no sexual
difficulties during the years of their
marriage before the onset of her illness but the
lack of sexual interest by the husband had
become increasingly evident during the
previous decade. His loss of sexual desire
did not, for example, extend to looking
at other women he considered attractive nor
to masturbating several times each
week when he was alone. He could not
explain his diminished sexual interest in his
wife. He clearly proclaimed his continuing
love for her and his feeling that her
sexual liaisons with other men held little
meaning.
Terminology
Various words and phrases are
used as synonyms for sexual desire, including libido,2
interest, drive, appetite, urge,
lust, and instinct. Low sexual desire is variously referred
to as: “sexual apathy,” “sexual
malaise,” and “sexual anorexia”3 (p. 315).
For consistency
with the DSM system and the
wording in most literature sources, the term “sexual
desire” is used here.
Problems In The Definition Of Sexual Desire
Sexual desire disorders are
enigmatic and difficult to know how to approach therapeutically,
and the entire concept of sexual
desire provokes some critical questions,
as follows:
• What is “normal” sexual desire?
Is it on a bell-shaped curve where, like
height or weight, some people
have a lot, some people have a little, and
most people are in the middle?
Kinsey and his colleagues attempted to
answer this question in saying “.
. . there is a certain skepticism in the
profession of the existence of
people who are basically low in capacity
to respond. This amounts to
asserting that all people are more or less equal
in their sexual endowments, and
ignores the existence of individual
variation. No one who knows how
remarkably different individuals may
be in morphology, in physiologic
reactions, and in other psychologic
capacities could conceive of
erotic capacities (of all things) that were
basically uniform throughout a
population”4 (p. 209). Zilbergeld and
Ellison suggest that “To say that
there is more or less of something
. . . necessitates a standard of
comparison . . . But there are no
standards of sexual desire; we do
not know what is right, normal, or
healthy, and it seems clear that
such standards will not be forthcoming”5
(p. 67). In a clear and
practical, but somewhat contrary, statement,
LoPiccolo & Friedman offered
the view that “In actual clinical practice
. . . most cases [of sexual
desire disorders] are so clearly beyond
the lower end of the normal curve
that definitional issues become
moot”6 (p.
110).
• Is sexual desire the same for
men as for women? Bancroft thought not.
He speculated “that there may be
a genuine sex difference in hormonebehavior
relationships, with men showing
consistent androgen/behavior
relationships across studies
(particularly androgen/sexual interest relationships),
whereas in women ‘the evidence
for hormone-behavior relationships
is much less consistent, and
often seemingly contradictory’.”7
• Does one measure sexual desire
subjectively (by thoughts and feelings),
or objectively (by actions), or
both? Considering only sexual actions or
behavior ignores the fact that,
sometimes, nonsexual motives govern
sexual activity. For example, a
person might engage in sexual
activity to please a partner,
quite apart from satisfying their own
feelings of sexual desire.
• Should sexual desire disorders
be classified as sexual dysfunctions
as they are in DSM-IV?8
Are they really on the same level
as, for example, physiological
difficulties such as erection and
orgasm problems, or do they
represent a totally different category
of sexual disorders? Some
patients distinguish the two by
Some patients explain that (1) erection
and orgasm problems are like automobile
engine troubles and (2) that desire
difficulties are more like a problem with
the starter in that the engine simply
does not turn over.
|
using the ubiquitous North
American symbol of the car, explaining that
erection and orgasm problems are
like engine troubles, whereas a desire
difficulty is more like a problem
with the starter in that the engine simply
does not turn over.
Classification Of Sexual Hypoactive Desire
Disorders
Disorders of sexual desire are
classified in DSM-IV as “Sexual Desire Disorders.”
(SDD).8 This
category contains two conditions:
• Hypoactive Sexual Desire
Disorder (HSDD or HSD)
• Sexual Aversion Disorder (SAD)
DSM-IV-PC summarizes the criteria
for the diagnosis of HSD as: “persistently or
recurrently deficient (or absent)
sexual fantasies and desire for sexual activity that
causes marked distress or
interpersonal difficulty” (p. 115), and criteria for SAD as:
“(A) persistent or extreme
aversion to, and avoidance of, any genital contact with
a sexual partner, causing marked
distress or interpersonal difficulty” and “(B) the
disturbance does not occur
exclusively during the course of another mental disorder
. . .”9(p.
116).
The separation of SDDs into two
groupings began with DSM-III,10 and while
Sexual
Aversion Disorder has received
some attention in the literature, it has not been the
subject of much research.9
HSD, the focus of this chapter,
is often not clinically distinguished from other
problems with sexual function
seen in primary care settings. Separating the two phenomena
and determining the chronology of
appearance (i.e., whichever developed
first) may be extremely important
clinically in considering etiology and treatment.
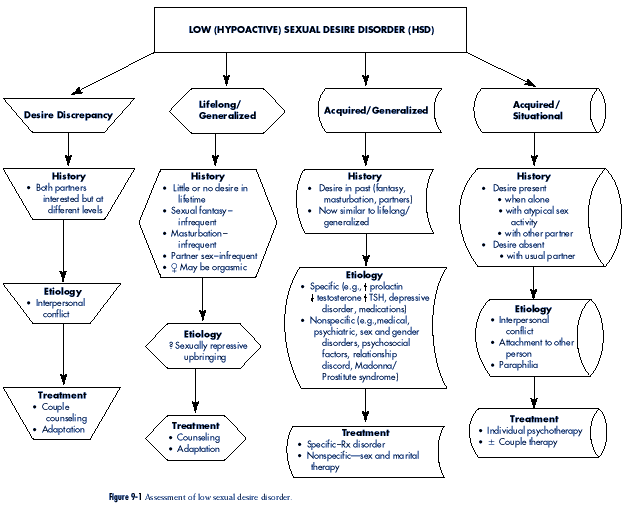
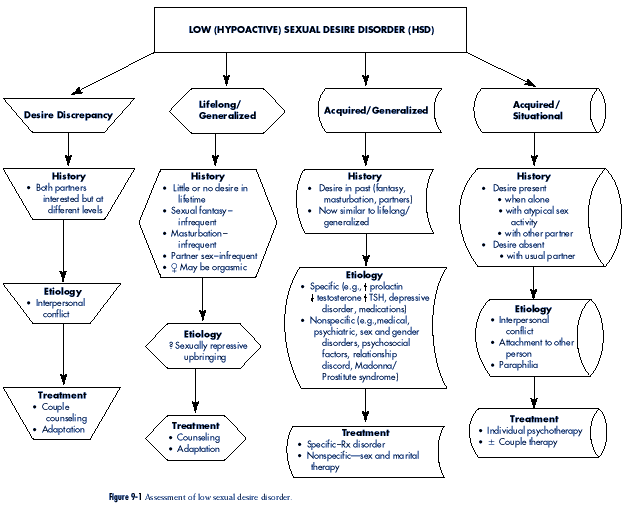
The assessment of low sexual
desire is outlined in Figure 9-1.
Subclassification Of Hypoactive Sexual Desire
Disorders: Descriptions
Sexual Desire Discrepancy
Although not categorized as a
“disorder” in DSM-IV8 or DSM-IV-PC,9
one of the ways that a sexual
desire problem becomes apparent is when
two partners are sexually
interested but not at the same level. Identical
levels of sexual desire in sexual
partners rarely occur. More usual is the
fact that both are interested but
one person is more interested than the
other. Couples generally “work
out” different sexual appetites by mutual
acceptance and compromise (or
“negotiation”). “Such discrepancies have much in common
with other relationship
difficulties—how to raise children, how often to dine out
or have company in, where to
spend the vacation, etc. . .”5 (p. 68).
Occasionally, a desire
discrepancy becomes a problem so that it results in a concern
brought to a health professional.
Couples sometimes focus on sexual problems as a way
of obscuring other tensions, but
then the history of the couple relationship should
indicate a change in sexual
interest. If the history of discrepancy dates from early in
the relationship (not necessarily
the beginning when “limerance” (see p. 182) may be
prominent), one has to ask: why
is it that these two people are unable to do what most
Identical levels of sexual desire in two
people rarely occur. Usually both are
interested but one person is more
interested
than the other. Couples generally
“work out” different sexual appetites by
mutual acceptance and compromise (or
“negotiation”).
|
couples seem to do, that is,
accept one another and compromise? The search for the
answer should begin on a primary
care level.
A couple in their mid-50s wanted assistance
because of a difference in sexual desire.
In talking with them initially together,
they candidly said that this discrepancy
existed since they married 30 years ago and
both agreed that her desire always had
been greater than his. When seen alone, he
elaborated on his initial statements by
saying that, indeed, there had always been
a difference in the amount of sexual
activity that each preferred. However, he
had not been candid with her in the past
about particular sexual practices which he
fantasized about and, in fact, had enjoyed
with other partners before they married. He
anticipated resistance from her in telling
her now, but, in fact, found the opposite.
The quality of their sexual experiences
improved greatly in the following months,
even though the quantity changed
little. When seen in follow-up six months
later, the issue of a sexual desire discrepancy
had not disappeared but there was much less
concern.
Lifelong and Generalized Absence of Sexual Desire
From a clinical viewpoint, this
particular form of sexual desire disorder seems to be
found more frequently in women
than men. The patient shows little, if any, indication
of sexual appetite in thought,
feeling, or action, now or in the past. Sexual experiences
with a partner occur uncommonly
and usually on the initiative of the other person.
The patient participates out of
recognition of the partner’s sexual needs rather than a
fulfillment of her own. Vaginal
lubrication and orgasm may occur but these are not
considered momentous.
Masturbation to the point of orgasm might also occur occasionally
but without enthusiasm. The
motivation for masturbation is often other than
sexual, such as wanting to
diminish feelings of anxiety or as an aid to inducing sleep.
Sexual dreams and fantasies are
nonexistent and the patient may describe a response to
romantic stories
in books or movies but not a response to depictions of sexual activity
in either. During adolescence,
the women thought of herself as different from girlfriends
in not being interested in boys,
easily fending off sexual propositions, and
hardly ever thinking about
anything sexual. She sums up her present status by saying
that she could live the rest of
her life without “sex,” and may add that the only reason
she is seeking consultation is
that, implicitly or explicitly, the viability of her relationship
is in jeopardy.
A 27-year-old woman was engaged for six
months and considering marriage. She
was concerned about her lack of sexual
interest and wondered if there was something
wrong with her. Primarily, she wanted to
know if anything could be done to
alter her present sexual situation. She
experimented sexually to the point of intercourse
on two occasions in the past and had become
sexually involved with her
husband-to-be shortly after they met. It
was apparent that she found these experiences
to be neither pleasurable nor repellent.
As a teenager she wondered what other girls
found so interesting about boys.
Sexual urges were not present then or
since. Her interest and energy was directed
toward scholastic studies, at which she
excelled. She eventually became a successful
lawyer, specializing in corporate law.
In a separate interview, her fiancee
indicated that while sexual experiences were
important to him, he was not willing to
forsake the relationship because of this
difficulty. In the one-year follow-up
interval, they married, and while her sexual
desire had not changed, she was active from
time-to-time as she sensed an increase
in his sexual needs. He preferred more sexual
activity but he felt as though they
had adapted in other ways.
Acquired and Generalized Absence of Sexual Desire
The major difference between the acquired
and generalized form of a sexual desire disorder
and the lifelong and
generalized form is that the present status represents a considerable
change from the past. In the
acquired and generalized form of HSD, the
patient describes having been
sexually interested and active in the past, but relates
much the same feelings about
“sex” in the present as the person with the lifelong form.
That is, she says that in
contrast to the past she does not now have sexual thoughts,
fantasies, or dreams and is only
infrequently sexually active with a partner or by herself
through masturbation. She may
also say that her interest level is such that life without
“sex” does not represent a
problem to her directly, although the opposite is usually true
for her partner.
A 47-year-old woman, married for 23 years,
described feeling diminished sexual
desire since her hysterectomy five years
earlier. She never experienced sexual difficulties
before. Medical history revealed that she
had the surgery because of excessive
menstrual bleeding associated with
fibroids: her ovaries were also removed and
she was on hormone replacement therapy (not
including testosterone) since then.
Intercourse continued after her
hysterectomy but what she liked most was the
closeness and affection that was part of
this experience. She had little problem
becoming vaginally wet when stimulated but found
that intercourse ceased to be
sexually gratifying. She was regularly
orgasmic in the past but was not so in the
present. Vaginal pain with intercourse
rarely occurred but when it did it was
momentary and disappeared with change in
position. Testosterone was given
because of her ovariectomy (see below) and
she found that, as a result, her sexual
desire was substantially enhanced.
Acquired and Situational Absence of Sexual Desire
The most striking feature that
differentiates a situational desire disorder from one that is
generalized is
the continued presence of sexual desire. The sexual feelings that do exist
in the present occur typically
when the person is alone and manifest either in thought
and/or action (through
masturbation), rather than in sexual activity with the patient’s
usual partner. The patient
characteristically states that there are sexual themes in his or
her thoughts and fantasies, and
perhaps attraction to people other than the usual partner.
Sexual activity with their
partner is considerably less frequent than sexual thoughts
in general. In addition, the
present level of sexual activity often represents a substantial
change from the beginning of the
relationship when the frequency was much greater.
However, as one reviews other
relationships in the past, it may become evident that
the same sequence of events
occurred before. That is, the interviewer might discover
that there was a pattern of
initial sexual interest in a partner, followed by a gradual
diminution of sexual interest,
resulting in relative sexual inactivity.
The 24-year-old wife of a 29-year-old man
described a concern about her husband’s
lack of sexual attention to her. They were
married for two years. When they first
met, she was relieved and pleased to find
that she did not have to fend him off
sexually and that he was quite prepared to
proceed at her pace. When asked about
their premarital sexual experiences with
one another, she related having had intercourse
on many occasions but also thought that she
was probably more sexually
interested than he.
After their marriage, the frequency of
sexual events dropped precipitously. Her
overtures were regularly turned aside, to
the point where she stopped asking. She
wondered whether his lack of interest was a
result of her becoming less sexually
appealing to him. When seen alone it became
clear that far from being sexually
neutral, and unknown to his wife, he
masturbated several times each week while
looking at magazine pictures of nude women.
Significant issues in the history of his
family-of-origin suggested that psychotherapy
would be the preferred treatment for this
man and he was subsequently
referred to a psychiatrist. He accepted
this outcome but when they were seen six
months later in follow-up he had a myriad
of reasons for not having followed
through on the referral. She was
disappointed at the turn of events, but not surprised.
When she then voiced her thoughts about
leaving him, he became more
determined to put aside his reticence to
seek assistance.
Epidemiology Of Hypoactive Sexual Desire
Disorder
Lack of sexual desire, or sexual
disinterest, is probably the most common
sexual complaint heard by health
professionals. Studies of the frequency of
sexual disorders tend not to
distinguish the different subcategories of
desire disorders, so that
separation into syndromes which are lifelong,
acquired, situational or
generalized are often based more on clinical
experience than research.
The survey completed by Laumann
and his colleagues was particularly
revealing about the subject of
sexual interest in the general population (as distinct
from specialty clinics).12
Interviewers asked respondents: “During the last 12 months
has there ever been a period of
several months or more when you lacked interest in
Lack of sexual desire, or sexual
disinterest,
is probably the most common sexual
complaint heard by health professionals.
|
having sex?” Overall, 33% of
women and 16% of men answered ‘yes.’
The most striking data concerning
women revealed that 40% to 45%
who were separated, black, did
not finish high school, and “poor”
answered positively (i.e., lacked
sexual interest). The equivalent data
concerning men were that 20% to
25% who were in the age group
50-59, never married, black, did
not finish high school, and “poor” also
answered positively. Positive
responses were also related to physical
health: women and men in “fair”
health, 42% and 25% respectively.
Fifty eight percent of women in
“poor” health, reported lacking sexual interest. These
numbers provoke one to think
about the definition of “normal” sexual interest and the
apparent role of social,
educational, and health factors in influencing sexual desire.
Frank and her colleagues’
impressive study of “normal” couples found a rate of sexual
“disinterest” almost identical to
the overall figures reported by Laumann et al12:
35% of
wives and 16% of husbands.13
In one specialty clinic, the
frequency of presentation of low-desire problems rose
from about 32% of couples in the
mid 1970s to 55% in the early 1980s6 (p. 112).
In
these same couples, the sex ratio
changed so that in the mid-70s, the woman was the
identified patient about 70% of
the time; in the early 80s, the man was the focus of
concern in 55% of cases. The
authors summarized the reason for this shift as follows:
“Women’s greater comfort with
their own sexuality allows them to put sufficient pressure
on their low-drive husbands to
get the couple into sex therapy; this was not true
until the woman’s movement
legitimized female sexuality.”
In a report on the frequency of
HSD in a population recruited for a study of sexual
disorders generally, 30% of the
men had HSD as a “primary” diagnosis.14 The same
authors described the frequency
in women as similar to that reported by others: between
30% and 50%, although they found
the figure to be 89% in their own study. Over one
third of the women and almost one
half of the men with a “primary” diagnosis of HSD
had another sexual disorder as
well. The authors concluded the following:
1. HSD was much more common in women
than men
2. Men with HSD were
significantly older than women
3. Desire disorders usually
coexist with other sexual dysfunctions
Little empirical information
exists on the epidemiology of specific HSD syndromes.
Among men, Kinsey and his
colleagues described 147 men (from about 12,000 interviewed)
as “low-rating” (defined as under
36 years of age and whose “rates” [of sexual
behavior] averaged one event in
two weeks or less4 (p. 207). Another group of
men,
about half the number, were
described as “sexually apathetic” in that “they never, at any
times in their histories, have
given evidence that they were capable of anything except
low rates of activity” (p. 209).
About 2% of women interviewed (of almost 8000) had
never by their late 40s
“recognized any sexual arousal, under any sort of condition”12
(p. 512).
On the basis of experience in
clinical settings that specialize in the assessment and
treatment of sexual problems, the
lifelong and generalized form of HSD seems very
unusual; the acquired and generalized
form appears to be the most common among
women. Within men who present
with HSD, the acquired and situational form seems
to be the most usual.
Interviewers asked respondents: “During
the last 12 months has there ever been
a period of several months or more
when you lacked interest in having
sex?” Overall, 33% of women and 16%
of men answered ‘yes.’
|
Components Of Sexual Desire
Attempts to understand the nature
of sexual desire (other than desire disorders) have
been elusive throughout history. In
modern times, Levine conceived of sexual desire as
having three parts16:
1. Sexual drive: “a
neuroendocrine generator of sexual impulses [that is] . . . testosterone-
dependent . . .”
2. Sexual wish: “a
cognitive aspiration [that] . . . emphasizes the purely ideational
aspect of sexual desire . . . The
most important element . . . is the willingness
to have sex [which, in turn] . .
. is a product of psychological motivation.”
(An example of a reason why a
person would be sexually willing, is to feel connected
to another person and less alone.
An example of the opposite is, because
the person may not yet like
anyone enough.)
3. Sexual motive: a factor
“that depends heavily on present and past interpersonal
relationships. [And which] . . .
seems to be the most important element of
desire under ordinary
circumstances” (examples of contributors to sexual motivation
include the quality of the
nonsexual relationship and sexual orientation)
Hormones And Sexual Desire
Biological factors represent one
vital component in the understanding of sexual desire
generally (in contrast to
disorders of sexual desire). Within the biological domain,
knowledge of the hormonal
influence on sexual desire is clearly critical—if for no
other reason than that many
people in the general population firmly believe that alterations
in hormones explain changes in
sexual behavior. Although this relationship is
unequivocally true in
subprimates, this view minimizes the huge impact of social learning
in humans. The enormous quantity
of literature on the significance of hormones on
sexual desire in men and women
was comprehensively reviewed by Segraves, from
which much of the information
included immediately below was taken.17
Men
Much of the evidence concerning
the connection between sexual desire
and hormones in men derives from
situations that involve decreased
androgens resulting from surgical
and chemical castration, aging, and
hypogonadal states. Surgical
castration results in a typical sequence of
changes: a sharp drop in sexual drive,
subsequent loss of the ability to
ejaculate, and then a lessening
of sexual activity. Regarding the effect
of testosterone loss on erections
(see Chapter 11), “It appears that
erectile problems are secondary
to a decrease in libido and not due to
a specific effect of androgen
withdrawal on the erectile mechanism”17
(p. 278). Chemical castration
mimics this lack of effect on erections.
In a study of aging,
testosterone, and sexual desire, Segraves observed
that while there is “ . . . a
strong relationship between aging and
libido, the relationship between
libido and androgen activity (in aging
men) was low, suggesting that
nonendocrinological factors may explain
Surgical castration results in a typical
sequence of changes: a sharp drop in
sexual drive, subsequent loss of the
ability to ejaculate, and then a lessening
of sexual activity.
“It appears that erectile problems are
secondary to a decrease in libido and
not due to a specific effect of androgen
withdrawal on the erectile mechanism”17
(p. 278).
|
the decline in sexuality with
aging”17(p. 281). Examples of nonendocrine factors
include:
• Marital boredom
• Diminished partner
attractiveness
• Chronic illness
In hypogonadal states, one can
witness the effect of testosterone deficiency
and subsequently the changes that
take place with recovery when
a replacement hormone is given.
“The clinical literature is consistent in
demonstrating a marked reduction
in libido and sexual activity in
untreated hypogonadal men”17(p.
281). To the extent that the provision
of androgens is successful in
hypogonadal men, evidence strongly suggests
a primary effect on sexual desire
rather than on erectile capacity.
The “impotence” that is seen in
hypogonadal men can be explained as
“performance anxiety” superimposed
on a biogenic desire disorder.
Studies of the treatment of
hypogonadal men show that the sexual
benefits of replacement
testosterone disappear as the normal range of
blood values is approached,
indicating the clinically vital suggestion
that treating men who have normal
testosterone levels for problems
relating to sexual responsivity
is likely to be ineffective. In fact, studies
of men who have normal levels
of testosterone but who are given an extra
amount for the treatment of
sexual difficulties suggest that “ . . . the
effects are subtle and of small
magnitude if they exist at all”17 (p. 284).
Elevated prolactin levels also
reveal significant information about
hormones and sexual desire in men
(and women). One study demonstrates
the futility of attempting to
strictly separate sexual problems of
“organic” and “psychogenic”
etiology.18 All of the hyperprolactinemic
men described difficulties with
sexual desire, as well as erection and/or
ejaculation dysfunction. Of
particular significance is that some of the
sexual problems of the men in
this group appear as situational difficulties
(e.g., dysfunction exacerbated by
psychological factors, which
improved at times of enhanced
arousal). Furthermore all of the men experienced
some improvement with sex therapy,
which was provided before the hyperprolactinemia
was discovered.
Women
Two areas of investigation help
in understanding the influence of hormonal factors on
sexual desire in women:
• The impact of endogenous
hormones (e.g., changes during the menstrual
cycle and with menopause)
• The effect of exogenous
hormones (e.g., oral contraceptives)
The possibility that sexual
interests change during the menstrual cycle precipitated
attempts to discern a
relationship between estrogens and progesterone and sexual
activity. A correlation has not
been found but some evidence shows that average serum
testosterone levels across all
phases are related to sexual responsivity17 (p.
290).
The impotence that is seen in hypogonadal
men can be explained as “performance
anxiety” superimposed on a biogenic
desire disorder.
An attempt to strictly separate sexual
problems into “organic” and “psychogenic”
etiology may be an exercise in
futility. In one study, all of the men with
hyperprolactinemia described difficulties
with sexual desire, erection, and/or
ejaculation dysfunction. Of particular
significance is that some of the sexual
problems appeared as situational
difficulties.
Also, all of the men experienced
some improvement with sex therapy,
which was provided before the hyperprolactinemia
was discovered.
Studies of men who have normal levels
of testosterone but who are given an
extra amount for the treatment of sexual
difficulties suggest that “. . .the
effects are subtle and of small magnitude
if they exist at all”17
(p. 284).
|
Changes in sexual desire
associated with menopause have also been investigated.
“A minority of women report some
decline in sexual activity . . .”17 (p. 295)
but this
could relate to factors other
than libido (e.g., health and attractiveness of the woman’s
partner). Some
psychophysiological studies report little or no change in subjective
sexual arousal of postmenopausal
women. Again, in contrast to naturally occurring
menopause, Sherwin and her
colleagues demonstrated that diminished sexual
desire and sexual fantasy
accompanies early menopause resulting from surgical removal
of a woman’s ovaries.19
The explanation for this observation appears to be decreased
testosterone associated with
ovariectomy. She also found that in about 50% of
instances of naturally occurring
menopause, the ovary continues to secrete testosterone;
in the other 50%, testosterone
secretion is negligible. She suggests the inclusion
of testosterone in replacement
hormones after a surgically induced menopause, and
also that, when diminished sexual
desire occurs coincidentally with naturally occurring
menopause, it might be reasonable
to add testosterone to an estrogen replacement
regimen (see “Treatment of
Hypoactive Sexual Desire Disorder” below).20
On the subject of the impact of
oral contraceptives on sexual desire, “The evidence
is unclear, but it does not
suggest that [they] have a marked effect on libido apart from
other side effects” such as
nausea and dysphoria17 (p. 292). Segraves
suggests the following
guidelines when faced with a
patient using oral contraceptives and complaining
of low sexual desire:
1. If diminished sexual desire
and other side effects persist beyond the second
month of use, it might (by
implication) be reasonable to change the preparation
2. If diminished sexual desire is
a solitary complaint and began after the initiation
of oral contraceptive use, it
might be sensible to have a trial period off
medications
3. If sexual desire returns “off
medications,” suggest a different drug
Etiologies Of Hypoactive Sexual Desire
Disorder
When considering sexual desire
difficulties (rather than sexual desire),
it seems best to think of these
problems as representing a “final common
pathway”6 (p.
116). The linguistic homogeneity implied by the specific
diagnosis of “Hypoactive Sexual
Desire Disorder” covers a great deal of
etiological heterogeneity. There
is no reason to assume that (1) HSD in
men arise(s) from the same
source(s) as in women, (2) a lifelong pattern
is caused by the same problems as
those which are acquired, or (3) a
situational disorder has the same
genesis as the other two. Although
HSDs in men and women are now
usually considered separately, the
same cannot always be said of
other subcategories.
The following were noted in a
descriptive examination of differences
in men and women seen in a “sex
clinic” with a sexual desire complaint21:
1. Men were described as
significantly older (50 years old versus 33)
2. Women reported a higher level
of psychological distress, although both groups
focused more on the sexual desire
concern
When considering sexual desire difficulties
(rather than sexual desire), it seems
best to think of these problems as
representing
a “final common pathway”6
(p. 116). The linguistic homogeneity
implied by the specific diagnosis of
“Hypoactive Sexual Desire Disorder”
covers a great deal of etiological
heterogeneity.
|
3. Men’s desire difficulties
seemed less affected by relationship discord or dissatisfaction
4. Women reported more domestic
stress
Generalized HSD
Biologically related studies of
HSD undertaken by Schiavi, Schreiner-Engel, and their
colleagues are at the forefront
of investigations into the etiologies of HSD and represent
important exceptions to the
heterogeneity described above. A controlled investigation
was completed on a group of men
who demonstrated a “generalized and persistent lack
of sexual desire” but who were
otherwise healthy.22 The HSD men were found to
have
significantly lower total plasma
testosterone levels when measured hourly throughout
the night. (The determination of
free testosterone did not show differences between the
HSD men and the controls). When
Nocturnal Penile Tumescence (NPT) comparisons
were made between the HSD men who
did and did not have additional erectile difficulties,
those who did showed a marked
depression in NPT activity when compared to
controls in duration, frequency,
and degree. The authors speculated that low sex drive
results in impaired NPT or that
both result from some central biological abnormality.
A companion study of women with
generalized HSD (lifelong [38%] and acquired)
who were otherwise healthy found
no significant differences from controls on hormonal
measures (including testosterone)
determined over the menstrual cycle.23 “It is
impressive that these two groups
of women, who differed so markedly in their levels
of sexual desire, had endocrine
milieus so similar.” The authors summarized by saying
that this and other studies
failed “to provide convincing evidence that circulating testosterone
is an important determinant of
individual differences in the sexual desire of
eugonadal women.”
Medical Disorders and HSD
Many medical conditions are
associated with a loss of sexual desire. These are summarized
in Box 9-1.
As described in Chapter 8, sexual
problems that are in general associated with medical
conditions arise from a variety
of sources. A loss of sexual desire in particular can
be a result of biological,
psychological, or social and interpersonal factors24 (pp.
356-366). Examples of biological
factors include the following:
1. Direct physiological effects
of the illness or disability
2. Direct physiological effects
of medical treatment and management (e.g., steroid
treatment of rheumatoid
arthritis)
3. Physical debilitation
4. Bowel or bladder incontinence
Examples of psychological factors
include:
1. Adopting the “patient” role
(as an asexual person)
2. Altered body image
3. Feelings of anxiety,
depression, and anger
4. Fears of death, rejection by a
partner, or loss of control
5. Guilt regarding behavior
imagined as the cause of a disease or disability
6. Reassignment of priorities
Box 9-1
Common Medical Conditions That May Decrease Sexual Desire
A DISEASES THAT CAUSE
TESTOSTERONE DEFICIENCY STATES IN
MALES:
castration, injuries to the testes,
age-related atrophic testicular degeneration, bilateral
cryptorchism, Klinefelter’s syndrome,
hydrocele, varicocele, cytotoxic chemotherapy,
pelvic radiation, mumps orchitis,
hypothalamic-pituitary lesions, Addison’s disease, etc.
Conditions requiring anti-androgens drugs,
e.g., prostate cancer, antisocial sexual
behavior, etc.
IN FEMALES:
Bilateral salpingo-oophorectomy,
adrenalectomy, hypophysectomy, cytotoxic chemotherapy,
hypothalamic-pituitary lesions, Addison’s
disease, androgen insensitivity
syndrome, etc.
Conditions requiring anti-androgen drugs,
e.g., endometriosis, etc.
B CONDITIONS THAT CAUSE
HYPERPROLACTINEMIA:
pituitary prolactin-secreting adenoma,
other tumors of the pituitary, hypothalamic
disease, hypothyroidism, hepatic cirrhosis,
stress, breast manipulation, etc., and conditions
requiring Prl raising medication, e.g.,
depression, psychosis, infertility, etc.
C CONDITIONS THAT DECREASE
DESIRE VIA UNKNOWN MECHANISMS:
hyperthyroidism, temporal lobe epilepsy,
renal dialysis, etc.
D CONDITIONS THAT CAUSE ORGANIC
IMPOTENCE (Indirect cause of low
sexual desire in men):
diabetes mellitus, arteriosclerosis of
penile blood vessels, venus leak, penile muscular
atrophy, Peyronie disease, Lariche’s
syndrome, steal syndrome, sickle cell disease, priapism,
injury to penis, etc.
E CONDITIONS THAT CAUSE
DYSPAREUNIA (Indirect cause of low sexual
desire):
IN FEMALES:
urogenital estrogen-deficiency
syndrome—normal age-related menopause, surgical
menopause, chemical menopause, irradiation
of ovaries; endometriosis, pelvic inflammatory
disease, vaginitis, herpes, vaginismus,
cystitis, etc.
IN MALES:
herpes, phymosis, post-ejaculatory
syndrome, etc.
F ALL MEDICAL CONDITIONS THAT
CAUSE CHRONIC PAIN, FATIGUE,
OR MALAISE (Indirect cause of
low desire):
arthritis, cancer, obstructive pulmonary
disease, chronic cardiac and renal insufficiency,
shingles, peripheral neuropathy, trigeminal
neuralgia, chronic infections, traumatic injuries,
etc.
(Modified from Kaplan HS: The sexual
desire disorders, New York, 1995, Brunner/Mazel, p. 286. Reprinted with
permission.)
|
Examples of social and
interpersonal factors include:
1. Communication difficulties
regarding feelings or sexuality
2. Difficulty initiating “sex”
after a period of abstinence
3. Fear of physically damaging an
ill or disabled partner
4. Lack of a partner
5. Lack of privacy
Gynecologic and urologic
disorders have a particular association with HSD. Testicular
and ovarian disorders can have
direct effects on sexual desire (see previous section
in this chapter on “Hormones and
Sexual Desire” and “Treatment of Hypoactive
Sexual Desire” below). Indirect
effects on sexual desire can also result from structural
disorders occurring in both body
systems. Given the fact that one of the major functions
of both the gynecologic and
urologic systems is sexual, it is hardly surprising that
when one function goes awry,
sexual function goes awry as well. This may easily result
in the patient being discouraged
and experiencing a concomitant (but secondary) loss
of sexual desire.
Hormonal Disorders and HSD
(See previous section in this
Chapter on “Hormones and Sexual Desire” and “Treatment
of Hypoactive Sexual Desire
Disorder” below.)
Psychiatric Disorders and HSD
The relationship between
psychiatric disorders and loss of sexual desire has not been
so carefully studied as loss of
sexual desire with medical disorders. On a clinical basis,
it seems that the association
between the two is exceedingly frequent. Of all psychiatric
disorders in which a loss of
sexual desire is an accompaniment, depression has
unquestionably received most
attention. Other aspects of depression have been scrupulously
scrutinized in the past but this
has been only recently true of its sexual ramifications.
The twin issues of depression and
sexual desire were carefully studied
in 40 depressed men before and
after treatment that did not include antidepressant
drugs (thus avoiding the
potentially confusing factor of the
effect of medications).25
Contrary to the expected diminution in sexual
desire, the authors found that
the initial level of sexual activity engaged in
by the subjects was not different
than the controls. The sexual behavior of
those subjects whose depression
remitted with treatment, did not change,
but what was altered was
the level of satisfaction derived from sexual experiences.
They concluded that“ . . . the
traditional notion of loss of sexual
interest in depressed outpatients
is not manifested behaviorally, but rather
reflects the depressed patient’s
cognitive appraisal of sexual function as
less satisfying and pleasurable.”
When subjects who did not remit, or only
partially remitted, were included
in the analysis, there was a “modest”
improvement in the level of
sexual activity and “drive.” The authors found the variability
of sexual function in depressed
men in this study particularly interesting.
Schreiner-Engel and Schiavi
looked at the association of psychiatric disorders and
low sexual desire from a
different perspective and found that HSD patients (men and
the sexual behavior of the subjects
whose depression remitted with treatment
did not change but what was
altered was the level of satisfaction
derived from sexual experiences.
Investigators
included that “. . . the traditional
notion of loss of sexual interest in
depressed outpatients is not manifested
behaviorally, but rather reflects the
depressed patient’s cognitive appraisal
of sexual function as less satisfying and
pleasurable.”25
|
women) had significantly elevated
lifetime prevalence rates of affective disorder compared
to controls.26
None of the patients or controls had a diagnosable illness at the
time of the study and there were
no differences found in lifetime diagnoses of anxiety
or personality disorders. In 88%
of the HSD men, and all of the HSD women, loss of
sexual interest occurred at the
time of, or following, the onset of the initial episode of
depression. The authors
speculated on the possibility that central monoaminergic processes
were involved in both HSD and
depression.
Medications and HSD
The influence of drugs looms
large among the various biological factors that can negatively
influence sexual desire. This
subject has been reviewed in detail by Segraves who
acknowledges the limitations in
information that often exists,3 such as:
1. Bias due to dependence on case
reports and questionnaire studies
2. Inconsistent use of
terminology
3. A focus on the sexual function
of men (and relative neglect of women)
4. Reliance on volunteered
(rather than requested) information about sexual sideeffects
5. Lack of clarity about effects
on different phases of the sex response cycle
Drugs that are said to cause HSD
are noted in Appendix III and Box 9-2.
Drug-related information seems to
change more rapidly than any other material in
health care; thus new drugs are
promoted for old diseases and side-effects of older
drugs become more apparent. The
result of the rapid pace of change in information
about sexual side effects of
drugs is the requirement that health professionals remain
informed. An example of this
change is the appearance of a negative impact on sexual
desire of the Selective Serotonin
Reuptake Inhibitors (SSRIs).27
Other Sexual and Gender Identity Disorders and HSD
Other sexual and gender identity
disorders may be associated with a loss of sexual
desire. Of particular
significance is the simultaneous occurrence of another sexual dysfunction
that may be a cause or a result
of HSD. Determining the order of appearance
of the two problems is crucial.
If the other sexual function difficulty preceded the loss
of sexual desire, successful
treatment of the former would likely result in disappearance
of the latter.
A couple in their late 20s and married for
five years was referred because the
woman was sexually disinterested. Detailed
inquiry of this complaint revealed that,
unknown to her husband, she regularly
fantasized about sexual activity and masturbated
to the point of orgasm using a vibrator
several times each month. Her lack
of sexual desire was specific to sexual
activity with her husband and dated from
about two years before. In the first three
years of their marriage, both freely initiated
sexual activity and she usually become
highly aroused but never reached the
point of orgasm. She became physically and
psychologically uncomfortable, so
much so that she decided that “it was
better not to start what (she) couldn’t finish.”
By her own description, she refused to
become aroused at the beginning of their
sexual encounters by deliberately “turning
off” her sexual desire. Her husband was
relieved to discover her interest in
masturbation and that she was orgasmic. He was
eager to find ways in which that experience
could be incorporated into their lovemaking
as a couple.
Box 9-2
Commonly Used Pharmacologic Agents That May Decrease Sexual
Desire
A ANTI-ANDROGEN DRUGS*:
Cyproterone* and Depo-provera* (for sex
offenders), Flutamide* (for prostate cancer
in men, virilizing syndromes in women,
precocious puberty in boys, etc.), Lupurin,* a
gonadotropin releasing hormone analog (for
prostrate cancer, used together with Flutamide,
also for endometriosis in women); cytotoxic
chemotherapeutic agents* (Adriamycin,
Methotrexate, Cytotoxin, Fluorouracil,
Cisplatin, etc.)
B PSYCHOACTIVE DRUGS:
1. Sedative-Hypnotics: loss of
desire dose-related: in low doses, disinhibition may cause
increase in desire; high doses and chronic
use reduce desire. Alcohol; Benzodiazepines
(Valium, Ativan, Xanax, Librium, Halcion,
etc); Barbiturates (phenobarbital, amytal,
etc.); Chlorol hydrate, Methaqualone, etc.
2. Narcotics* (Heroin, Morphine,
Methadone, Meperidine, etc.)
3. Anti-Depressants: (Dopamine
blocking and serotonergic) SSRIs* (Prozac, Zoloft,
Paxil); Tricyclics (Tofranil, Norpramin,
Amitriptyline, Aventyl, Clomipramine*); MAOIs*
(Nardil, Marplan), Lithium carbonate, Tegretol.
4. Neuroleptics (increase Prl): Phenothiazine
(Thorazine,* Thioridazine) Prolixin,* Stelazine,
Mellaril, etc.); Haldol,* Sulpiride.*
5. Stimulants: loss of desire is
dose-related: low, acute doses may stimulate libido; high
doses and chronic use reduce sex drive.
(Dexadrine, Methamphetamine, Cocaine).
C CARDIAC DRUGS:
1. Antihypertensives: (Hydrochlorothiazide,*
Chlorthalidone,* Methyldopa,*
Spironolactone,* Reserpine,* Clonidine,
Guanethidine,* etc.)
2. Cardiac Drugs: Beta adrenergic
blockers* (Inderal, Atenolol, Timolol, etc.); Calcium
blockers** (Nifedipine, Verapramil, etc.)
D DRUGS THAT BIND WITH
TESTOSTERONE:
1. Tamoxifen, Contraceptive agents, etc.
E MISCELLANEOUS DRUGS: Cimetidine*
(for peptic ulcer); Pondimin* (serotonergic
appetite suppressor); Diclorphenamine,
Methazolamide (for glaucoma); Clofribrate,
Lovastatin (anticholesterol); Steroids
(chronic use for inflammatory conditions),
(Prednisone, Decadron, etc.).
*All the drugs listed have been reported to
result in the loss of sexual desire and/or in erectile problems. However, the
frequency with which sexual side effects
occur varies considerably, and the drugs that have a very high incidence of
decreased libido have been marked with*.
**Long-acting calcium channel blockers are
more likely to decrease desire and impair erection than the short-acting
preparations.
(Modified from Kaplan HS: The sexual
desire disorders, New York, 1995, Brunner/Mazel, p. 287. Reprinted with
permission.)
|
Psychosocial Issues and HSD
Psychosocial causes of low sexual
desire include the following6 (pp.
119-129):
1. Religious orthodoxy (a factor
that is “oversimplified at best”)
2. Anhedonic or
obsessive-compulsive personality style (accompanied by usual
difficulties of displaying
emotion and discomfort with close body contact)
3. Primary sexual interest in
other people of the same sex
4. Specific sexual phobias or
aversions (after sexual assault as an adult or child28)
5. Masked paraphilia (perversion)
6. Fear of pregnancy
7. “Widower’s syndrome” (sexual function
difficulties, usually in the areas of desire
or erection, in a man after his
wife has died, resulting from attachment to his
wife or the unfamiliarity of
sexual activity with a new partner)
8. Relationship discord (cause,
effect, or coexistence with HSD may be difficult
to determine)
9. Lack of attraction to a
partner
10. Poor sexual skills in the
partner (“lousy lover”)
11. Fear of closeness and
inability to fuse feelings of love and sexual desire (especially
in men [see “Acquired and
Situational Absence of Sexual Desire”
above])
Relationship Discord and HSD
On the basis of clinical
impression, relationship discord and HSD seem to be frequently
related to each other. When two
sexual partners who love each other and
have no sexual concerns
are engaged in a dispute, it is commonplace to declare a
sexual moratorium until the
conflict resolves. It is as if one says to
the other, ‘I’m angry at you and
don’t feel like going to bed with
you while I have these feelings’.
It is logical to theorize that some
instances of acquired HSD that
are nonspecific in origin may represent
submerged anger about which the
person is unaware. Experimental
evidence exists for the idea of
suppressed sexual desire in the
presence of anger.29
Such theorizing may provide direction for clinical
care. This observation about
anger may, in some instances, relate
to the finding that when woman
with and without HSD were compared, the former
“reported significantly greater
dissatisfaction with nearly every reported relationship
issue.”30
In the concluding chapter to
their multi-authored book on the subject of Sexual
Desire Disorders, Leiblum and
Rosen summarized the views of contributors generally,
saying that “ . . . relationship
conflicts are viewed by the majority of our contributors
as the single most common cause
of desire difficulties”31 (p. 452).
From personal clinical
experience, they found that women
partners “were more aware of and less willing
to tolerate relationship
distress, and consequently that desire in women is more readily
disrupted by relationship
factors” (p. 449). At the same time, humility was suggested
with treatment because
all-too-often less marital discord resulted without any accompanying
change in sexual desire (p. 451).
It is logical to theorize that some
instances of acquired HSD that are
nonspecific
in origin may represent submerged
anger about which the person is
unaware.
|
Madonna/Prostitute Syndrome and HSD
Freud described a man choosing
one woman for love and another for sexual activity
and seemingly unable to fuse the
two.2 He referred to this idea as the Madonna/
Prostitute syndrome. It seems
especially applicable today to many young men who
relate experiences consistent
with an acquired and situational form of HSD.
Multiple Etiological Factors in HSD
Sometimes HSD seems to result
from the operation of only one of the factors described
above: a hormone deficiency or
the onset of a debilitating illness. More often than not,
the onset (especially of the
acquired form) can probably best be explained by multiple
factors.32
A couple in their late 20s explained that
during the two years before their marriage
and the three years before she became
pregnant their sexual experiences were
mutually initiated, frequent, pleasurable,
and free of problems. After the delivery of
her child, attempts at intercourse were
painful for her. Her husband knew of this
but persisted in approaching her sexually.
After telling him of her discomfort on
one occasion, she felt she had little
alternative but to “put up with it,” until finally
she became quite disinterested and “shut
down.”
Both partners described her as a person who
could not candidly and frankly talk
about her feelings, especially when she was
angry. Being forthright was discouraged
in her family-of-origin, particularly by
her alcoholic father who was verbally
abusive to her when she said something he
found unpleasant. It seemed that the
current sexual difficulties were
superimposed on some issues concerning her personality
and problems in their relationship as a
couple. The treatment program
centered on her expressiveness, as well as
“communication” and sexual issues. Her
ability to talk openly about her feelings
improved dramatically. Her husband was
upset with himself as he discovered the
extent of her vaginal and psychological
discomfort and his own insensitivity. As
their sexual experiences resumed, she discovered
that her dyspareunia disappeared. However,
although lovemaking was
more frequent than before, her previous
sexual urge did not return.
Investigation of Hypoact
ive Sexual Desire Disorder
Given the etiological
heterogeneity and therapeutic complexity of
HSD, careful investigation of the
complaint and establishing the correct
subcategory is often the most
important contribution that can be
made by a primary care physician.
Scrutinizing the history of the
patient and couple is usually the most
revealing part of the
examination. Concerns about sexual desire usually
surface in the context of a
couple’s relationship. The patient often
appears unruffled, and the
partner seems the one who is more distressed.
The patient becomes upset
secondarily if the partner is implicitly or
explicitly threatening to
dissolve the relationship. Sexually interested
Given the etiological heterogeneity and
therapeutic complexity of HSD, careful
investigation of the complaint
and
establishing the correct
subcategory is
often the most important
contribution
that can be made by a primary
care clinician.
|
women who are partners of
disinterested men may also describe doubts about themselves
and wonder if they are the source
of the difficulty, thinking (for example) that
they are sexually unappealing.
The disinterested person often does not express worry
about himself or herself but more
about the unfulfilled sexual needs of the partner.
Occasionally, the disinterested
partner seeks help. The reason is often a feeling of
sexual abnormality because such
patients compare themselves, for example, to (1) how
they felt in the past, (2)
friends and partners, and (3) depictions of “sex” on TV and the
movies.
Complaints about sexual desire
are infrequent in patients without partners. One
exception is when a person
believes that their lack of sexual interest contributed to a
disrupted previous relationship
and is apprehensive about it happening again.
History
Comprehensive assessment of a
complaint about sexual desire involves asking an initial
open-ended question, followed by
specific inquiry concerning at least three areas:
• Sexual behavior
• Psychological manifestations of
sexual stimuli
• Body changes in response to
sexually arousing stimuli
Specific issues to inquire about,
and suggested questions include the following:
1. Duration (see Chapter 4,
“lifelong versus acquired”)
Suggested Question: “Has a
feling of low sexual desire always
ben part of your life or was
there a time when this was not
a problem?”
2. Sexual behavior with the usual
partner (see Chapter 4, “generalized versus
situational”)
Suggested Question when Talking
with a Heterosexual Man/Woman: “About how
often are you and she/he sexualy
involved with each
other?”
Additional Suggested Question
when Talking with a Heterosexual Man/Woman:
“What kind of thoughts do you
have before or during your
sexual experiences?”
3. Sexual behavior with other
partners of the opposite sex (see Chapter 4, “generalized
versus situational”)
Suggested Question: “Have you
had sexual experiences with other
women/men since you’ve ben in
this relationship ?”
4. Sexual behavior with other
partners of the same sex (see Chapter 4, “'Generalized
versus situational”)
Part II
Sexual Dysfunctions in Primary Care: Diagnosis, Treatment, and
Referral 178
Suggested Question: “Are you
sometimes sexualy aroused by
thoughts of other men/women?
Additional Suggested Question if
the Answer is, “yes”: “Apart from thoughts,
have you had sexual experiences
with other men/women?”
5. Sexual behavior through
masturbatory sexual activity (see Chapter 4, “generalized
vs. situational”)
Suggested Question: “How
frequently do you stimulate yourself
or masturbate ?”
6. Psychological
manifestations—fantasy (see Chapter 4, “generalized versus situational”)
Suggested Question: “How often
do you have sexual daydreams
(or fantasies )?”
Additional Suggested Question: “What
do you fantasi ze about when
masturbating ?” ALSO:
“What do you fantasi ze about when
you’re in the midst of a sexual
experience with another
person
?”
7. Psychological
manifestations—response to pictures with a sexual theme (see
Chapter 4, “generalized versus
situational”)
Suggested Question: “What do
you think about and fel sexualy
when you se a picture or movie
that has a sexual theme?
8. Psychological
manifestations—response to stories in literature (see Chapter 4,
“generalized versus situational”)
Suggested Question: “What do
you think about and fel sexualy
when you read story in which
something sexual ocurs?”
9. Body change—genital swelling
[erection or vaginal lubrication] (see Chapter 4,
“description”)
Suggested Question when Talking
with a Man/Woman: “When you think about
something sexual, what hapens to
your penis/vagina ?”
Additional Suggested Question: “Does
it become hard/do you become
wet?”
10. Psychological accompaniment
(see Chapter 4, “patient and partner’s reaction to
problem”)
Suggested Question: “When you
are sexualy uninterested, what
thoughts are going through your
mind?”
Addition Question: “How does
your wife (husband, partner )
react?”
Patients who regard answers to
questions about sexual desire as private should not
be expected to discuss these
aspects of the topic (at least initially) in the presence of
their partner (see Chapter 6).
When a couple is interviewed together and someone is
asked a question about something
generally regarded as private, the fact of not answering
the question might, itself, be
revealing (i.e., if one partner does not want to answer
a question about masturbation,
the non-answer might convey to the other partner that
there is secret information).
Under such circumstances, it is best to avoid the question
altogether. The clinician must be
careful not to unwittingly coerce someone to disclose
private information to a partner.
Information that was obtained when someone was
seen alone may emerge at a later
time when a couple is seen together but this should
occur only if the patient who previously
asked for privacy takes the initiative.
Questions about thoughts and
sexual fantasies (with masturbation or with a partner)
are often regarded by patients as
even more private than actual behavior. As a result,
there may be obvious reticence to
talk about what occurs in one’s mind. Information
about thoughts and sexual
fantasies can be enormously revealing from a diagnostic
point of view, since it may, for
example, indicate a complete absence of sexual thought,
a sexual desire for someone else,
or, a different sexual orientation than what the person’s
behavior may have suggested.
Physical Examination
The potential significance of the
physical examination in HSD is signaled by the
patient’s history. Considering
the four subcategories described above,
the acquired and generalized loss
of sexual desire is the principal form
in which a diagnostic physical
examination is required. The major
contrasting element separating
the acquired/generalized pattern from
the others is widespread change.
Ordinarily one would not expect to
find physical abnormalities with
the other three forms because of the
absence of such change:
discrepancy in sexual desire, as well as situational
and lifelong/generalized
disorders. With a desire discrepancy, interest continues
to exist by both partners in the
present as it was in the past, but it is nevertheless
problematic because the two
people function at different levels. Where sexual desire
is situationally absent, interest
continues as before except for one particular situation.
In the lifelong/generalized form,
if a physical abnormality existed it would also have
been lifelong, a circumstance
that is possible (e.g., a congenital disorder) but at the
same time usually obvious.
If a physical examination is part
of the evaluation of acquired and generalized loss
of sexual desire, what does one
look for? Before attempting to answer this question,
one must ask what loss of sexual
desire represents. Is it, in fact, a disorder? Or is it a
syndrome (a collection of
symptoms resulting from several causes)? In most instances,
the answer seems to be the
latter. In that sense, loss of sexual desire resembles other
phenomena such as loss of
appetite for food, or fatigue (both are accompaniments of
many different medical and
psychiatric disorders from cancer to depression and neither
are associated with any specific
physical findings on examination).
The acquired and generalized loss of
sexual desire is the principal form in
which a diagnostic physical examination
is required.
|
When the complaint is loss of
sexual desire and the history does not suggest a specific
cause, one looks for evidence of
generalized and previously unrecognized disease
(e.g., renal or cardiac disease)
in a physical examination. One would search also for the
physical changes associated with
abnormalities in endocrine function. The main endocrine
disorders would be hypoandrogen
states and hypothyroidism. Physical signs of
low testosterone in men are often
delayed; in women, they are often absent. Signs of
hypothyroidism may be subtle.
Since generalized disease and endocrine disorders can
coexist, the presence of the
former does not necessarily mean that the explanation for
sexual desire loss has been found
and that a search for an accompanying endocrine
disorder is, therefore,
unnecessary.
Laboratory Studies
Since HSD is occasionally a
result of a hormonal deficiency, laboratory studies usually
become part of the evaluation
process. In men, this should always involve a determination
of the patient’s serum
testosterone and prolactin levels. Segraves17 (p.
285) justifies
this policy in the following
ways:
• Low cost
• Possibility of overlooking
treatable cause of a low desire complaint
• Difficulty in distinguishing
psychological from endocrinological causation
on the basis of history alone
• Negligible risk (i.e.,
venipuncture)
He further emphasizes the
importance of too quickly attributing the cause of low
desire to interpersonal discord,
since low sexual desire may, itself, result in relationship
conflict. In an effort to
determine the cause of a low testosterone level and because of
the negative feedback loop in
relation to the pituitary gland, a follow-up test should
be performed to determine the
patient’s Luteinizing Hormone (LH) status. Other clinicians
propose a somewhat different
format. Kaplan suggests that LH testing should
coincide with testing for
testosterone, free testosterone, prolactin, total estrogens, and
thyroid status (for men)33
(p. 289). Kaplan, and Rosen & Leiblum, suggest that Follicle
Stimulating Hormone (FSH) be
measured as well.32,33
On the subject of laboratory
investigation of sexual desire complaints in women,
Segraves suggested that “ . . .
extensive endocrinological assessment of every case
of inhibited sexual desire in
females is not indicated”17 (pp.
298-99). He adds that,
since many gynecological
conditions may interfere with sexual desire in nonspecific
ways (e.g., causing dyspareunia),
correction of the condition may be sufficient to
reverse the sexual problem. As
well, low sexual desire might occur in postmenopausal
women as a result of
uncomfortable or painful intercourse associated with the
diminished vaginal lubrication.
This symptom commonly accompanies atrophic vaginitis
and is caused by lack of estrogen
stimulation to a woman’s vagina (see Chapter
13). The unusual patient with the
complaint of diminished sexual desire but who
also describes absent menstrual
periods and galactorrhea should have a serum prolactin
determination test performed.
Kaplan differed from Segraves in suggesting
that the hormone profile
described in the previous paragraph be used in women as
well as men; the one exception
being that estradiol be determined instead of total
estrogens33 (p.
289).
Unrecognized, untreated, or
uncontrolled medical and psychiatric disorders may
become evident during the
investigation of a sexual problem. Common sense dictates
that, ordinarily, attention to
the sexual problems be delayed until these other disorders
are under control. Examples
include the following6:
• Depression
• Alcohol or drug dependence
• Spouse abuse
• Active extramarital
relationships
• Severe marital distress with
imminent separation or divorce
Treatment of Hypoactive
Sexual Desire Disorder
In many circumstances, the most
important role of the primary care health professional
is to carefully delineate the
subcategory of desire difficulty and the possible
etiology. While
carrying out this task, patients with HSD, regardless
of cause, will usually appreciate
the primary care clinician’s initial
step of encouraging them to agree
to temporarily stop struggling
with attempts at sexual
experiences (no matter how favorable the circumstances)
and to simply enjoy being affectionate
with their partner.
The history of the couple often
reveals that affectionate exchanges were common
in the past but abandoned with
the onset of the desire difficulties, since affection
was interpreted as a prelude to
an unwanted (and often refused) sexual encounter.
Affection without the “threat” of
any sexual consequence is usually a relief and
something that is highly desired
by the disinterested partner. This arrangement is
easily accomplished in primary
care, and the agreement is best made with both
partners together so that there
is no misinterpretation of directions or mutual
blame.
Specific Treatment Approaches
Specific treatment of a sexual
desire disorder will result from the discovery of a
specific cause. Limits to the
involvement of a particular health professional depends
on that person’s skills and
pattern of practice. An illustration of a specific cause is
that of testosterone deficiency.
For example, Sherwin showed that testosterone is
beneficial in the loss of sexual
desire associated with surgically induced menopause
as a result of bilateral
oophorectomy.19 Also, testosterone may be helpful in
medically
induced menopause that results
from the use of some cytotoxic agents and
radiation in treatment of various
cancers.34-36 A second and more complex example
of a specific etiology is the
discovery and treatment of prostate cancer. In this
instance, sexual counseling has a
major role in program of care and would likely
focus on “here-and-now” issues.
The treatment program may involve the coordinated
work of a nonpsychiatric
physician and sex-specialist or mental health professional
with interest and skills in the
area of sexual rehabilitation. A third and potentially
even more intricate example of a
specific cause is loss of sexual desire after
Patients with HSD usually appreciate the
primary care clinician’s initial step of
encouraging them to temporarily stop
struggling with attempts at sexual
experiences
and to simply enjoy being affectionate
with their partner.
|
sexual trauma. Counseling is
pivotal in treatment and might well extend to past
issues in the patient’s life. The
ongoing care of such a patient would optimally be
undertaken by a health care
professional with psychotherapy skills and comfort in
talking about sexual issues.
Nonspecific Treatment Approaches
Nonspecific methods for the
treatment of a sexual desire disorder must be used if, as is
often the case, specific
explanatory factors cannot be pinpointed. Some clinicians and
patients find that self-help
books are useful in the initial care of a patient with nonspecific
HSD.37 Unfortunately,
few such books exist.
The subcategory of HSD should be
considered in nonspecific treatment objectives
and methods.
Sexual Desire Discrepancy
Differences in sexual desire
among sexual partners are so common as to possibly be
universal. Considered from that
perspective, one might then consider such differences
to be “normal” rather than
“pathological.” The epidemiology of discrepancies in sexual
desire should be conveyed to
patients—not to delegitimize their complaint but to help
them understand that other
nonsexual issues may be significant contributors to the
problem.
Primary care health professionals
can assist partners in the following ways:
1. Understanding the role of
extraneous influences on their sexual experiences
(e.g., fatigue and preoccupation,
especially in relation to the parenting of young
children)
2. Talking candidly about the
sexual expectations that each may have of the other
3. Appreciating the significance
of “transition activities” (see following paragraph)
4. “Negotiating” a sexual
activity compromise
Even before attempting to alter
facets of sexual desire, attention should be paid to the
role of “transition activities”
(e.g., sporting activities or dinners alone). “It is no secret
that modern living produces
tremendous tension which often inhibits sexual interest,
excitement, and performance . . .
The type of transitions employed are of little
moment, the important thing being
that they help move [the patient] from a tense,
pressured state to one which
feels more comfortable and in which he or she is more
open to sexual stimuli . . . When
[transition activities] are done together [with a
partner], they can function as a
bridge into a shared building of arousal and enjoyable
sexual activity”5
(p. 95).
Viewing sexual desire
discrepancies in the same way as other relationship discrepancies
“ . . . suggests a focus on both
partners, rather than the more common practice
of working only on the partner
with less interest . . . we (try) to increase the desire
of the one while at the same time
trying to decrease that of the other”5 (p. 68).
Careful history-taking sometimes
reveals that a difference in sexual desire actually
represents a diminution on
the part of one partner. This apparent decrease may actually
represent a lowering of sexual
desire to the patient’s usual level after an initial period
of “limerance,” (the passionate
intensity of a new romantic relationship). A sexual
desire discrepancy may then
appear as a desire disorder that is acquired and generalized.
Lifelong and Generalized Absence of Sexual Desire
Altering a lifelong absence of
sexual desire is exceedingly difficult at any level of care,
primary or otherwise. If the
major treatment purpose is one of substantially enhancing
the patient’s level of sexual
desire, an approach at any level will likely, in ordinary
circumstances, not be productive.
However, one reasonable treatment objective is the
reversal of any concomitant
sexual dysfunction. For example, a woman patient with
this form of HSD may also be
anorgasmic. While becoming orgasmic may not result
in much change in her sexual
desire level, sexual events may become more pleasurable
for her and as a result cause
less tension in the couple’s relationship. (In instances of
low sexual desire, disappointment
usually follows an expectation that an improvement
in the quality of sexual
experiences results in an increase in the quantity). In the absence
of an associated sexual
dysfunction, treatment to help the couple adapt to this situation
could be potentially quite
beneficial. Even accomplishing this objective can be difficult
and time-consuming and is
probably best undertaken by a sex-specialist with counseling
skills, or a mental health
professional comfortable and skilled in talking about
sexual and relationship issues.
Acquired and Generalized or Situational Absence of Sexual
Desire
Psychological Treatment Methods
Nonspecific treatment methods for
HSD are usually psychologically based, involve
counseling or psychotherapy, and
involve individuals or couples. Techniques vary and
include:
• Psychodynamic and interpersonal
approaches16,39,40
• Cognitive and behavioral
methods6,41,42
• Systems and interactional
approaches43,44
Unfortunately, little consensus
exists concerning treatment approaches to nonspecific
HSD. Also, not all health
professional groups have the requisite interest, knowledge,
or training in the use of these
various treatment techniques. The situational absence of
sexual desire requires
psychologically-based treatment methods only.
Hormonal Treatment: Men
Hormonal treatments have been
used for nonspecific HSD. For example, some men
who complain of “impotence” have
an HSD rather than an erectile difficulty. Physicians
will sometimes attempt a trial of
testosterone for their male patients with the
general concern of “impotence”
without ascertaining whether a desire disorder exists
and is, in fact, primary.
Segraves is unequivocal in his opinion: “Some physicians routinely
prescribe exogenous testosterone
to men with sexual complaints without determining
baseline
values or even monitoring the
serum testosterone response to exogenous
androgens. There is little
justification for such an approach”17 (p. 288).
Beyond
this opinion, physicians must be
concerned about exogenous testosterone accelerating
the growth of an existing but
occult prostatic cancer or the risk of prostate cancer
development.45
Hormonal Treatment: Women
There is considerable controversy
over the use of androgens in the treatment of a
sexual desire disorder in
postmenopausal women. (Kaplan is adamant in saying that
testosterone “has no place in the
treatment of premenopausal women” (italics added) with
normal testosterone levels)33
(p. 278).
Other than specific research,
Sherwin speculates that testosterone may be helpful to
women who report diminished
libido beginning in the perimenopausal time period.20
Kaplan also suggests that
physiological doses (of testosterone) present little risk and
that “a brief trial is justified
in postmenopausal women with a global loss of libido
whose T (testosterone) levels are
abnormally low . . . or in the low-normal ranges. (She
considered 20-25 ng/dl to be the
lower limit of normal levels according to her clinical
experience and a survey of
medical texts)33 (p. 279).
In contrast to the encouragement
of Sherwin and Kaplan, Segraves regards the use
of testosterone in the care of
women with a sexual desire disorder to be “clearly experimental”
17 (pp. 294-5) and suggests
caution for the following reasons:
1. The studies have not been
properly controlled
2. Doses used exceed
physiological levels
3. Side effects can be unpleasant
4. There is lack of clarity about
the effect on sexual desire of variations in androgens
within the normal physiological
(versus subphysiological) range that women
experience
Others have also been circumspect
about promoting testosterone for the care of postmenopausal
women with a sexual desire
disorder because of evidence for its possible
role in the development of breast
cancer. Dorgan and her colleagues conducted a prospective
study that involved examining
blood that was donated up to 10 years before.
Women who subsequently developed
breast cancer (compared to healthy controls)
had significantly higher serum
levels of the adrenal androgens dehydroepiandrosterone
(DHEA), its sulfate (DHEAS), and
its metabolite 5-androstene-3b,17b-diol
(ADIOL).46,47
There is concern about the role
of sex steroids in the etiology of cardiovascular
disease in postmenopausal women,
particularly over the potentially negative effect of
testosterone on lipid levels.
Sherwin et al. reviewed the literature on this subject and
concluded that “the evidence that
testosterone decreases HDL (high density lipoprotein
cholesterol) and increases LDL
(low density lipoprotein cholesterol) is impressive.”
She nevertheless found a
different result in her own subjects.48 She
compared the
effect of different hormone
treatment approaches on the lipoprotein lipid profiles of
three groups of women who had
undergone total hysterectomy and bilateral salpingooophorectomy:
a combined estrogen-androgen
preparation (containing 150 mg of testosterone
enanthate), estrogen alone, and
an untreated group. She reported “no
between-group differences in
total cholesterol, triglycerides, high-density lipoprotein,
or low-density lipoprotein
values. Nor was the low density/high density lipoprotein
ratio significantly different
between groups. . . .”
Research findings on the effect
of testosterone on lipids in postmenopausal women
are contradictory. Phillips and
his colleagues found that free testosterone (in contrast
to total testosterone) was
significantly related (positively) with coronary artery disease
in a group of 60 postmenopausal
women undergoing coronary angiography.49 The
authors speculated that an
elevated free testosterone level might be a risk factor for
coronary atherosclerosis.
In her research on women who
experienced surgically induced menopause, Sherwin
considered the possibility of an
equal and opposite effect of each hormone (estrogen and
androgens) that masked the effect
of testosterone alone.48 Another
study found that
testosterone prevented (to a
small degree) the rise in HDL cholesterol
that was seen in oophorectomized
women given estrogen alone.50 The
same authors found in yet another
study that testosterone decreased
LDL cholesterol.51
The complexity of the issue was further illustrated by
the unpublished finding that
estrogen alone and estrogen-testosterone
implants resulted in lower LDL
and increased HDL cholesterol but that
estrogentestosterone implants in
heavy smokers produced a fall in HDL
cholesterol.52
Some speculate that the mode of administration of the
hormones may have a role in
explaining the contradictory findings.48
In summary, testosterone seems
beneficial to women with an androgen
deficit as a result of surgically
(and probably medically) induced
menopause and diminished sexual
desire. There is no reported evidence
that testosterone is useful in
the treatment of sexual desire difficulties
in men or postmenopausal women
who have experienced a naturally occurring menopause.
Some evidence exists that it may
be harmful.
Treatment Outcome
of Hypoactive Sexual Desire
Despite the enormity of the
problem of HSD in extent (in the general population) and
depth (in the individual), the voluminous
scientific literature on the subject, and the
many treatment approaches that
have been described (often with confidence in their
utility), there is not a great
deal of information concerning treatment results. The two
existing long-term follow-up
studies of treatment of low sexual desire are generally
quite discouraging. De Amicis et
al. found that three years after treatment, “desire for
sexual contact and frequency of
sexual contact, clearly demonstrate a lack of sustained
success for both men and women.”53
Despite the absence of change in the specific
problem, both men and women
reported continued improvement in “satisfaction in
[the] sexual relationship,” and
women also reported persistent improvement in the
“frequency of orgasm through
masturbation and genital caress.” Hawton et al. reported
on a prospective follow-up study
of sex therapy undertaken for various sexual disorders.
54 Treatment occurred between
one and six years earlier and at least one partner
was interviewed in 75% of cases. The
effects of treatment in instances of “female
impaired sexual interest,”
“showed a marked deterioration (italics added) . . . when compared
with post-treatment outcome. This
finding is accentuated by the fact that even
post-treatment outcome for this
problem was relatively modest.”
There are only a handful of
controlled treatment studies of HSD. O’Carroll reviewed
the only eight that he could find
that met his (gradually expanding) inclusion criteria
for his search.7
These included two psychotherapy studies, three drug or hormone
Testosterone seems beneficial to women
with an androgen deficit as a result of
surgically (and probably medically)
induced menopause and diminished sexual
desire. There is no reported evidence
that testosterone is useful in the
treatment
of sexual desire difficulties in men
or postmenopausal women who have
experienced a naturally occurring
menopause.
Some evidence exists that it may
be harmful.
|
studies, and three studies that
combined the two methods. Of this review, he concluded
that “if only studies which had
specified (and analyzed) a discrete subject group
who presented with low sex
interest had been accepted, one would have been left with
a single controlled treatment
study which used only ten subjects!”
The one study about which
O’Carroll wrote compared ten men with HSD to ten
men with erectile dysfunction.55
All initially had normal testosterone levels and all
were treated with high-dosage
testosterone or placebo using a double-blind crossover
design. The HSD men responded
with a significantly increased level of frequency of
sexual thoughts. O’Carroll
concluded that “high dosage testosterone treatment may
have a modest role to play in the
treatment of some eugonadal men who present with
low sex interest.”7
Leiblum and Rosen reviewed
factors associated with treatment outcome found by
those who presented case
histories in their multi-authored book “Sexual Desire Disorders.”
56 Success was particularly
linked (p. 453) to desire problems affecting men who
were in their 30s, 40s, and 50s
and who reported concomitant sexual dysfunctions
(especially erectile
difficulties) and, in the case of couples, commitment to the marriage
(despite relationship discord)
and the treatment process (p. 454). Unsuccessful
outcome of treatment was
especially evident (p. 454) when there were secrets in the
marital relationship, history of
chronic alcoholism, religious orthodoxy, history of
depression, organic erectile
dysfunction, and “major body image problems.”
Indications for Referral
for Consult ation or Continuing
Care by a Specialist
Etiological heterogeneity of HSD
means that therapeutic versatility is a necessity. The
required range of skills will not
likely be in the armamentarium of all primary care
clinicians. Referral may become
necessary and the kind of health professional to whom
a referral is made will depend on
the knowledge and skills of each and the apparent
cause of the disorder.
Specific Causes of HSD
The capabilities of the primary
care clinician may or may not encompass the treatments
required for patients with
specific causes of HSD. One or several visits with a consultant
from a different discipline may
be needed and may be all that is necessary. However, in
complex circumstances it may also
be advisable to complement one’s own care (over an
extended time period) with that
of another health professional who has different skills.
• One example of a specific cause
of HSD that sometimes requires only a
consultation is the diagnosis of
major depression. While most patients
with this diagnosis are entirely
cared for by primary care health professionals,
in some instances, physicians in
primary care might provide
antidepressant medication and
psychotherapy to the patient after consultation
and advice from a psychiatrist or
psychotherapist.
• Another example of a specific
cause of HSD that may require more than
simple consultation is the loss
of sexual desire associated with the diagnosis and treatment
of prostate cancer. This situation may require asking
the advice of a medical
specialist and the continuing cooperative efforts
of the primary care clinician and
a sex-specialist with counseling skills.
• A third example of a specific
cause of HSD that may involve ultimate
transfer of the patient to
another health professional is that of sexual
trauma (see “Sexual Sequelae of
Child Sexual Abuse in Adults: Sexual
Issues and Questions” in Chapter
8). A primary care professional may
provide acute care but the needs
of the patient may require ongoing
intensive care from a mental
health professional who has psychotherapeutic
skills and is also comfortable
with sexual topics.
Nonspecific Causes of HSD
The care of an individual or
couple where HSD is a concern, and for which no explanation
has become apparent after
investigation, reasonably suggests referral—at least
for brief consultation, and often
for continuing care. Despite the great frequency of the
problem in the general
population, nonspecific HSD is, generally, not a disorder amenable
to care at the generalist level. Careful
subclassification and investigation are the most
important responsibilities of the
primary care clinician when considering nonspecific HSD, and they will
determine the direction of
referral. In most instances, the most helpful professional is a sex
therapist or sexual medicine
specialist with counseling skills.
• Desire discrepancies
occasionally do not respond to intervention at the
primary care level. Consideration
might then be given to referral to a
mental health professional who is
also comfortable with couples and in
talking about sexual issues. Even
then, referral should probably be
reserved for circumstances that,
if they continue, may threaten the continuity
of the relationship.
• HSD that is lifelong and
generalized often presents with questions
about the continuity of a current
relationship. Care of the patient or
couple who appear in these
complex and potentially turbulent circumstances
should be undertaken by a sex
therapist or sexual medicine specialist
with a mental health professional
background.
• The acquired and generalized
form of HSD arises from several sources
(see above) and the apparent
origins (there may be more than one)
influence the direction of
referral. Because (1) the nature of such
complaints are perplexing and
intricate, (2) etiological clarity is often
lacking, (3) disappointment and
(often) anger is generated by the sexual
change, and (4) because the
partners are usually disappointed when
they discover that expectations
of return to previous sexual desire status
often is not realized, treatment
at the primary care level is not suggested.
In most instances sex therapists
or sexual medicine specialists,
should be involved in treatment,
at least on a consultation level if not
in the continuing care of such
individuals or couples.
• HSD that is acquired and
situational occurs for a multiplicity of reasons
and each one requires a different
referral approach. For example, some
instances are clearly a result of
relationship discord, and the appropriate
person to be caring for such a
couple would be a mental health professional
interested in relationship
therapy. Other instances may represent
a disorder such as the
Madonna/Prostitute Syndrome (discussed earlier
in this chapter), for which
treatment is quite intricate and warrants
referral to a mental health
professional for continuing care. Yet other
cases are a result of sexual
issues specific to a couple (e.g., odors) and in
that instance, should be referred
to a sex therapist.
Summary
The problem of low sexual desire
or Hypoactive Sexual Desire Disorder (HSD)
requires subclassification into
syndromes that denote at least four possibilities:
• A desire discrepancy
• A disorder that is lifelong and
generalized
• A disorder that is acquired and
generalized
• A disorder that is acquired and
situational
In general, low or absent sexual
desire is the most common sexual complaint heard by
health professionals, and about
one third of women and one sixth of men answering a
community survey report having
had this experience for several months during the last
year. Testosterone seems to be
the “libido hormone” for men and women in that withdrawal
of this substance has profound
effects on sexual desire in both. Elevated Prolactin
has a similar effect. HSD seems
to arise from many different sources, hence the
application of the term: final
common pathway. When compared to normal controls, biologically
related studies of healthy people
with HSD have found some testosterone
determinations and nocturnal
penile tumescence differences in men, but no differences
in women. HSD is associated with
the following:
• A variety of general medical
conditions
• Gynecologic and urologic
disorders
• Psychiatric disorders
• Substance abuse
• Other sexual and gender
identity disorders
• Intrapersonal difficulties
• Relationship discord
The investigation of HSD requires
history-taking, physical examination for generalized
disorders, and selective
laboratory studies. The most valuable contribution
of primary care professionals to
patients with HSD is correct subclassification and
investigation of the etiology.
Treatment of HSD depends on the reason for the
disorder. The more specific the
etiology, the more specific the treatment, and the
more specific the treatment, the
more might be reasonably undertaken in primary
care—alone or together with
another health professional. Nonspecific HSD (apart
from the problem of a desire
discrepancy) generally requires referral to a health
professional who specializes in
the counseling and therapy of people with sexual
difficulties.
REFERENCES
1. Levine SB: Sexual life: a
clinician’s guide, New York, 1992, Plenum Press.
2. Freud S: The transformations of puberty:
[3] the libido theory. In Freud S: On sexuality:
three essays on the theory of
sexuality and other works, Middlesex, 1905/1977, Penguin
Books,
pp. 138-140.
3. Segraves T: Drugs and desire. In Leiblum
SR, Rosen RC (editors), Sexual desire disorders,
New York, 1988, The Guilford Press, pp.
313-347.
4. Kinsey AC, Pomeroy WB, Martin CE: Sexual
behavior in the human male, Philadelphia and
London, 1949, W.B. Saunders.
5. Zilbergeld B, Ellison CR: Desire
discrepancies and arousal problems in sex therapy. In
Leiblum SR, Pervin LA (editors): Principles
and practice of sex therapy, ed 1, New York, 1980,
The Guilford Press, pp. 65-101.
6. LoPiccolo J, Friedman JM: Broad-spectrum
treatment of low sexual desire: integration of
cognitive, behavioral, and systematic
therapy. In Leiblum SR, Rosen RC (editors): Sexual
desire disorders,
New York, 1988, The Guilford Press, pp. 107-144.
7. O’Carroll R: Sexual desire disorders: a
review of controlled treatment studies, J Sex Res
28:607-624, 1991.
8. Diagnostic and statistical manual of
mental disorders, ed 4, Washington, 1994, American
Psychiatric Association.
9. Diagnostic and statistical manual of
mental disorders, ed 4, primary care version, 1995, Washington,
American Psychiatric Association.
10. Diagnostic and statistical manual of
mental disorders, ed 3, 1980, Washington, American
Psychiatric Association.
11. Kaplan HS: Sexual aversion, sexual
phobias, and panic disorder, New York, 1987, Brunner/
Mazel, Inc.
12. Laumann EO et al: The social
organization of sexuality: sexual practices in the United States,
Chicago, 1994, The University of Chicago
Press, pp. 35-73.
13. Frank E, Anderson C, Rubenstein D:
Frequency of sexual dysfunction in normal couples,
N Engl J Med 299:111-115,
1978.
14. Segraves KB, Segraves RT: Hypoactive
sexual desire disorder: prevalence and
comorbidity, J Sex Marital Ther 17:55-58,
1991.
15. Kinsey AC et al: Sexual behavior in
the human female, Philadelphia and London, 1953, W.B.
Saunders.
16. Levine SB: Intrapsychic and individual
aspects of sexual desire. In Leiblum SR, Rosen RC
(editors): Sexual desire disorders,
New York, 1988, The Guilford Press, pp. 21-44.
17. Segraves T: Hormones and libido. In
Leiblum SR, Rosen RC (editors): Sexual desire
disorders,
New York, 1988, The Guilford Press, pp. 271-312.
18. Schwartz MF, Bauman JE, Masters WH: Hyperprolactinemia and
sexual disorders in men,
Biol Psychiatry 17:861-876, 1982.
19. Sherwin BB, Gelfand MM, Brender W: Androgen enhances sexual
motivation in females:
a prospective, crossover study of sex steroid
administration in the surgical menopause,
Psychosom Med 47:339-351,
1985.
20. Sherwin BB: Menopause and sexuality, Can
J Obstet/Gynecol Women’s Health Care 4:254-260,
1992.
21. Donahey KM, Carroll RA: Gender
differences in factors associated with hypoactive
sexual desire, J Sex Marital Ther 19:25-40,
1993.
22. Schiavi RC et al: Pituitary-Gonadal
function during sleep in men with hypoactive sexual
desire and in normal controls, Psychosom
Med 50:304-318, 1988.
23. Schreiner-Engel P et al: Low sexual
desire in women: the role of reproductive hormones,
Horm Behav 23:221-234,
1989.
24. Bullard DG: The treatment of desire
disorders in the medically ill and physically
disabled. In Leiblum SR, Rosen RC (editors): Sexual
desire disorders, New York,1988, The
Guilford Press, pp. 348-384.
25. Nofzinger EA et al: Sexual function in
depressed men, Arch Gen Psychiatry 50:24-30,
1993.
26. Schreiner-Engel P, Schiavi RC: Lifetime
psychopathology in individuals with low sexual
desire, J Nerv Ment Dis 174:646-651,
1986.
27. Segraves T: Overview of sexual
dysfunction complicating the treatment of depression, J
Clin Psychiatry 10:4-10,
1992.
28. Becker JV: Impact of sexual abuse on
sexual functioning. In Leiblum SR, Rosen RC (editors):
Principles and practices of sex
therapy: Update for the 1990s, ed 2, New York, 1989, The Guilford
Press, pp. 298-318.
29. Bozman AW, Beck JG: Covariation of sexual
desire and sexual arousal: the effects of
anger and anxiety, Arch Sex Behav 20:47-60,
1991.
30. Stuart FM, Hammond DC, Pett MA: Inhibited
sexual desire in women, Arch Sex Behav
16:91-106, 1987.
31. Leiblum SR, Rosen RC (editors): Sexual
desire disorders, New York, 1988, The Guilford
Press.
32. Rosen RC, Leiblum SR: Hypoactive sexual
desire, Psychiatr Clin North Am 18:107-121,
1995.
33. Kaplan HS: The sexual desire disorders:
dysfunctional regulation of sexual motivation, New York,
1995, Brunner/Mazel.
34. Kaplan HS, Owett T: The female androgen
deficiency syndrome, J Sex Marital Ther
19:3-24, 1993.
35. Feldman JE: Ovarian failure and cancer
treatment: incidence and interventions for the
premenopausal woman, Oncol Nurs Forum 16:651-657,
1989.
36. Chapman RM: Effect of cytotoxic therapy
on sexuality and gonadal function, Semin Oncol
9:84-94, 1982.
37. Williams W: Rekindling desire: bringing
your sexual relationship back to life, Oakland, 1988, New
Harbinger Publications Inc.
38. Nichols M: Low sexual desire in lesbian
couples. In Leiblum SR, Rosen RC (editors):
Sexual desire disorders,
New York, 1988, The Guilford Press, pp. 387-411.
39. Scharff DE: An object relations approach
to inhibited sexual desire. In Lieblum
SR, Rosen RC (editors): Sexual desire
disorders, New York, 1988, The Guilford Press,
pp. 45-74.
40. Apfelbaum B: An ego-analytic perspective
on desire disorders. In Leiblum SR, Rosen RC
(editors), Sexual desire disorders,
New York, 1988, The Guilford Press, pp. 75-104.
41. Rosen RC, Leiblum SR: A sexual scripting
approach to problems of desire. In Leiblum
SR, Rosen RC (editors): Sexual desire
disorders, New York, 1988, The Guilford Press,
pp. 168-191.
42. Lazarus AA: A multimodal perspective on
problems of sexual desire. In Leiblum SR,
Rosen RC (editors): Sexual desire
disorders, New York, 1988, The Guilford Press,
pp. 145-167.
43. Schwartz MF, Masters WH: Inhibited sexual
desire: the Masters and Johnson Institute
treatment model. In Leiblum SR, Rosen RC
(editors): Sexual desire disorders, New York,
1988, The Guilford Press, pp. 229-242.
44. Verhulst J, Heiman JR: A systems
perspective on sexual desire. In Leiblum SR, Rosen RC
(editors): Sexual desire disorders,
New York, 1988 The Guilford Press, pp. 243-267.
45. Gann et al: Prospective study of sex
hormone levels and risk of prostate cancer, J Natl
Cancer Institute 88:
1118-1126, 1996.
46. Dorgan JF et al: Relation of
prediagnostic serum estrogen and androgen levels to breast
cancer risk, Cancer Epidemiol Biomarkers
Prev 5:533-539, 1996.
47. Dorgan JF et al: Relationship of serum
dehydroepiandrosterone (DHEA), DHEA sufate,
and 5-androstene-3b,17b-diol to risk of
breast cancer in postmenopausal women, Cancer
Epidemiol Biomarkers Prev 6:177-181,
1997.
48. Sherwin BB et al: Postmenopausal estrogen
and androgen replacement and lipoprotein
lipid concentrations, Am J Obstet Gynecol 156:414-419,
1987.
49. Phillips GB, Pinkernell BH, Jing T-Y:
Relationship between serum sex hormones and
coronary artery disease in postmenopausal
women, Arterioscler Thromb Vasc Biol 17:
695-701, 1997.
50. Farish E et al: The effects of hormone
implants on serum lipoproteins and steroid
hormones in bilaterally oophorectomized
women, Acta Endocrinol 106: 116-120, 1984.
51. Fletcher CD et al: Long-term hormone
implant therapy- effects on lipoproteins and
steroid levels in postmenopausal women, Acta
Endocrinol 111:419-423, 1986.
52. Sands R, Studd J: Exogenous androgens in
postmenopausal women, Am J Med 98(suppl
1A):76S-79S, 1995.
53. De Amicis LA et al: Clinical follow-up of
couples treated for sexual dysfunction, Arch Sex
Behav 14:467-489,
1985.
54. Hawton K: Long-term outcome of sex
therapy, Behav Res Ther 24:665-675, 1986.
55. O’Carroll R, Bancroft J: Testosterone therapy
for low sexual interest and erectile
dysfunction in men: a controlled study, Br
J Psychiatry 145:146-151, 1984.
56. Leiblum SR, Rosen RC: Conclusion:
Conceptual and clinical overview. In Leiblum SR,
Rosen RC (editors): Sexual desire
disorders, New York, 1988, The Guilford Press,
pp. 446-458.