CHAPTER 3
Screening For Sexual Problems
The most basic, and also most
difficult, aspect of studying sexuality is defining the subject matter.
What is to be included? How much
of the body is relevant? How much of the life span? Is sexuality
an individual dimension or a
dimension of a relationship? Which behaviors, thoughts, or feelings
qualify as sexual—an unreturned
glance? Any hug? Daydreams about celebrities? Fearful memories of
abuse? When can we use similar
language for animals and people, if at all?
Tiefer,
19951
Defining
the subject matter of “sex” is, indeed, difficult but nevertheless crucial,
since
its meaning will determine which
difficulties one is searching for in the process
of screening. The definition and
the screening mechanism must be broad enough to
encompass problems with sexual function
and sexual practices. Problems with sexual
function are reported by patients
rather than observed by health professionals. In
contrast, some sexual practices
may be seen only as problematic by health professionals.
In both instances, the onus
remains on the health professional to elicit the
information.
Problems with sexual function
have been classified in DSM-IV2—a system
heavily
influenced by the research of
Masters and Johnson3 and Kaplan’s revisions.4
On the
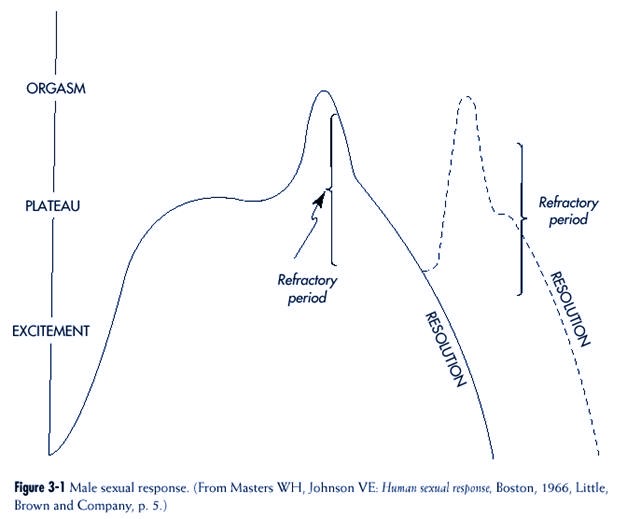
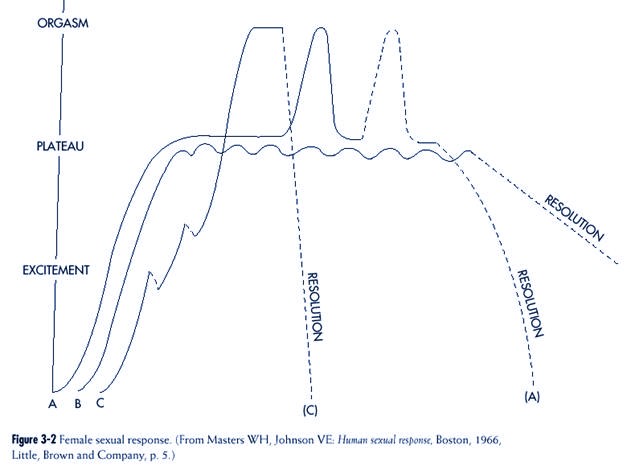
basis of direct observation of
physiological changes associated with sexual arousal,
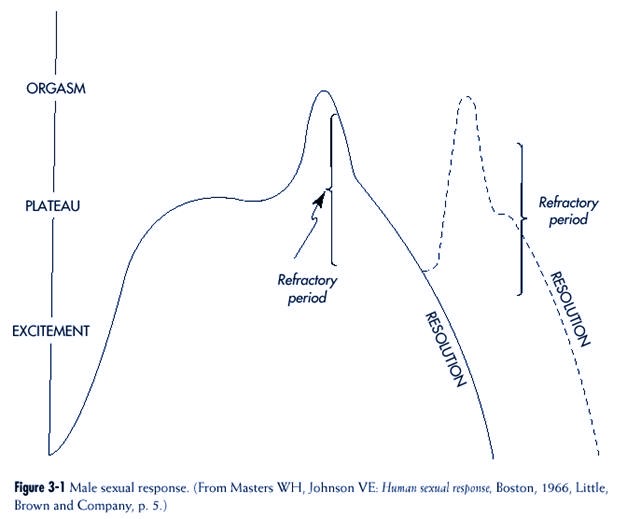
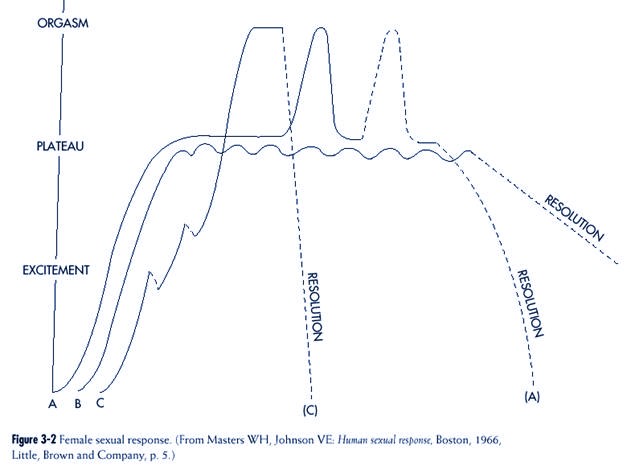
Masters and Johnson described a “sex
response cycle” that included four phases3 (pp.
3-8)
(Figures 3-1 and 3-2):
• Excitement
• Plateau
• Orgasm
• Resolution
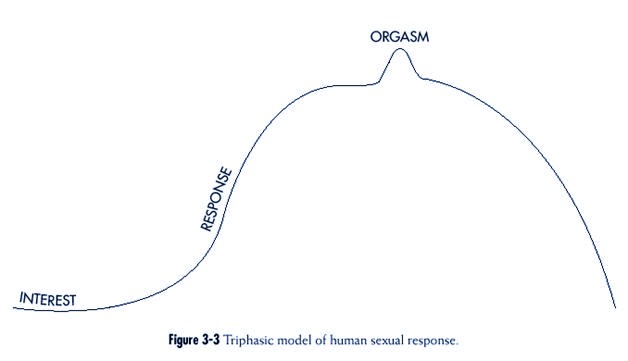
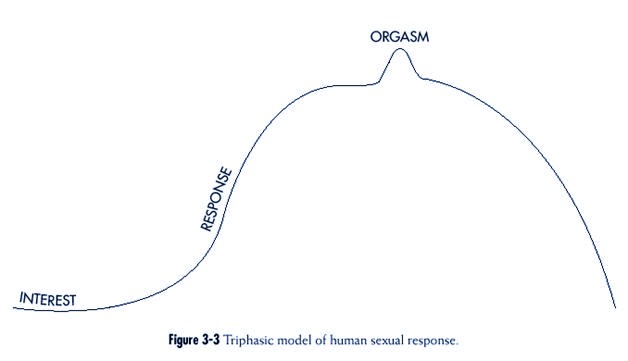
Kaplan added a prior “interest”
or motivational phase to Masters and Johnson’s system4
(pp. 3-7). In so doing, she
reconceptualized the sex response cycle from four parts into
three, which she renamed:
• Interest
• Response
• Orgasm
Kaplan referred to her revision
as a “triphasic model” (Figure 3-3).
Screening Content: Dysfunctions Versus Difficulties
While ideas based on the sex
response cycle are widely used, they have not been universally
accepted. One criticism is that
when considering sexual function, the cycle
seems to progress from one step
to another but that this is not how sexual response is
always ordered. For example,
clinicians will sometimes encounter the occurrence of
orgasm in a woman who does not
feel any preexisting sexual desire. The reality of this
particular observation of the disconnection
between desire and orgasm has been established
in a research context.5
A second critique relates to
gender and the different meanings of “sex” to men and
women. In an exquisitely detailed
and incisive analysis, Tiefer examined the entire
concept of the sexual response
cycle and the extent to which women have been absent
in the formulation of sexual
disorders in the various versions of the DSM1 (pp.
41-58, 97-102). She faults the
DSM classification system for the following:
1. Excessive “physiologizing”
2. Viewing sexual expression as
consisting of reactions of body parts
3. Being “genitally focused”
4. Thinking of “heterosexual
intercourse as the normative sexual activity, repeatedly
defining dysfunctions as failures
in coitus”
From Tiefer’s perspective, the
sexual concerns of women are different and have
been sufficiently outlined in
popular surveys, questionnaire studies, political writings,
and fiction to include such
issues as: intimacy, communication, emotion,
commitment, pregnancy, conception,
and getting old. “. . . women rate affection
and emotional communication as
more important than orgasm in a sexual relationship.
. . “1 (p.
56).
One well-executed, frequently
quoted, and revealing questionnaire study referred
to by Tiefer and which serves to
buttress her argument was conducted by Frank and
her colleagues.6
One hundred predominantly white, well-educated, and “happily
married”
volunteer couples were questioned
concerning the frequency of sexual problems.
The authors found that in addition
to the fact that 40% of the men and 63%
of the women reported sexual
dysfunctions, 50% of the men and 77% of the women
reported “difficulty that was
not dysfunctional in nature.” The “difficulties” are outlined in
Box 3-1. Most importantly from the
point of view of screening, the number of difficulties
reported was more strongly and
consistently related to overall sexual dissatisfaction than the number
of “dysfunctions.”
If one therefore accepts the argument and evidence presented by
Tiefer, a useful screening system
must consider sexual problems to be impairments in
physiology (sexual dysfunctions) and
impairments in the “human relations” part of
“sexual experiences” (i.e.,
difficulties or consequences of the ways people conduct
themselves sexually).
Epidemiology of Sexual
Problems in Primary Care
Apart from what one looks for in
screening (sexual “dysfunctions” and/or “difficulties”)
a major rationale for the inquiry
process is how common the detected phenomena are
in general (epidemiological information
about specific dysfunctions are included in
Part II). The extent of sexual
problems found in medical practices has been studied on
several occasions.
One widely quoted study of sexual
issues in general medicine practice was described
in detail in Chapter 1.7
Another study used a questionnaire (whose validity and reliability
was previously tested) that
contained items concerning dysfunctions and difficulties.
8 Of the 152 patients who
were asked to complete the questionnaire, almost all
did so (93%). The majority of
patients (56%) identified at least one sexual problem on
the questionnaire, and this
compared to 22% having a marital or sexual problem found
by simply examining the patient’s
medical record. Multiple reasons were cited for the
discrepancy, including:
1. The physician did not ask
relevant questions
2. The patient did not
spontaneously report problems
3. The physician did not record
the information in the patient’s
chart
Although identification of a
problem by 56% of patients may appear to
be an overwhelming number to a
clinician, one must remember that
not all people with sexual
problems want treatment.9
Box 3-1
Sexual “Difficulties”
• Partner chooses inconvenient time
• Inability to relax
• Attraction(s) to persons other than mate
• Disinterest
• Attraction(s) to persons of the same sex
• Different sexual practices or habits
• ”Turned off”
• Too little foreplay before intercourse
• Too little “tenderness” after intercourse
Adapted from Frank E et al: Frequency of
sexual dysfunction in “normal” couples,
N Engl J Med 299:111–115, 1998.
Although identification of a problem by
56% of patients may appear to be an
overwhelming number to a clinician,
one must remember that not all people
with sexual problems want treatment.9
|
Screening Criteria
Given the immense numbers of
patients with sexual problems, the need becomes obvious
for a triage system whereby the
nature of a problem and its impact can be evaluated
and proper action taken: (1)
further assessment and treatment or (2) referral. The
beginning of this process
requires a reasonable, respectful, and regular practice by
which the presence of sexual
problems can be identified with just a few questions. For
reasons discussed in Chapter 1,
it is a “given” that patients be provided the opportunity
to discuss a sexual issue if they
desire. To accomplish this goal, some sort of sexscreening
question must be included in an
assessment.
Other than considering specific
sexual practice issues involved in STD and HIV/
AIDS transmission, the idea of
including general sex-screening in a health assessment
has been considered only briefly
by a few authors. Concepts vary from an elaborate
“screening history” requiring 30
minutes10 to a small number of specific screening
questions.11The
rationale for choosing particular questions was not always clear.
Useful screening questions in any
area should observe at least four rules:
1. Screening questions should
encompass a wide spectrum of common problems
A variety of sexual problems may
exist in any community, ranging from frequent
(concerns about genital function,
sexual practices, or emotional communication) to
unusual (confusion about one’s
status as a man or woman). A screening system must be
sufficiently sensitive to at
least “pick up” problems that are common. Freund’s opinion is
that “a problem must be
sufficiently common to justify investigation of an entire population
of patients.”12
Sexual dysfunctions and difficulties, as well as problems related
to
STDs and child sexual abuse, are
far more numerous than other sexual disorders and
these must be uncovered in any
practical sex-screening process13 (pp.43-55).
2. To be practical, screening
questions should be few in number
A small number of questions
recognizes the limited amount of time
that health professionals
(especially nonpsychiatric physicians) spend
with patients and the reticence
that many patients have in spontaneously
talking about sexual issues.
Realistically and reasonably, only a
small amount of health
professional time will be used to ask questions
about sexual matters when the
patient’s major concern is elsewhere.
Suggesting more than a few
screening questions dooms the entire process
from the start.
3. The problem must be of
sufficient severity to justify the effort of asking questions of
the population12
The consequences of sexual
problems must be considered from individual and social
perspectives. In some instances,
the severity of the impact on an individual is easy to
discern (e.g., STDs) but in
others the effect may be more subtle (e.g., repercussions on
a relationship of a coexistent
sexual dysfunction). Without “quality of life” information
in the area of sexual problems,
it becomes difficult to provide clear evidence about the
effect of some problems on the
individual. The existing literature on the effects of
Realistically and reasonably, only a
small amount of health professional
time will be used to ask questions about
sexual matters when the patient’s major
concern is elsewhere. Suggesting more
than a few screening questions dooms
the entire process from the start.
|
sexual dysfunctions on
individuals and relationships, as well as clinical impression, suggest
substantial repercussions13
(pp. 52-55). The outcome of some sexual experiences
such as child sexual abuse are
well documented.14 Newspapers have well
reported the
social disruption caused by STDs
and HIV/AIDS, pedophilia, and child sexual abuse.
4. There must be effective
treatment for problems that are common
The treatments of sexual
dysfunctions and their usefulness are reviewed in Part II.
These four screening criteria can
be applied, for example, to one of the screening
systems commonly used in medical
practice. Part of any medical evaluation includes
asking a series of questions
about the function of different parts of the body. This brief
health questionnaire has been
variously called the “Review of Systems” (ROS) or “Functional
Inquiry” and includes a few
questions about each body system. It is meant to
accomplish two objectives, as
follows:
• To provide more information
about concerns not obviously connected
to the patient’s main complaint
• To uncover undiscussed problems
that the patient may have thought to
be irrelevant or unimportant
Until recently, questions about
sexual issues were not usually part of a medical
screening process. Questions
relating to this subject were not asked or were buried in
questions about other body
systems. For example, questions about sexual function
were included with questions
about a man’s urinary function.
There is no universally
applicable sex-screening formula. Several
approaches can be used,
depending, for example, on such factors as the
comfort and skill of the
interviewer or the age of the patient. Screening
questions asked of adolescents
might well differ from questions asked
of elders.
With the understanding that variety
and flexibility in sex screening are
desirable, one general method is
described below. This approach can
be incorporated easily into the
assessment of any patient whose main concern is not
primarily sexual, specifically,
into the medical “review of systems.” (The ROS concentrates
on body function or dysfunction;
therefore sexual practice issues can be included
easily.) When judging the
usefulness of the proposed sex-screening process, one should
recall the four criteria
mentioned previously, that is, questions should:
• Cover a wide spectrum of common
problems
• Be few in number
• Justify the severity criterion
• Be concerned with problems that
have effective treatments
Questions should include an
additional criterion as well, namely, practicality.
When health professionals choose
sex-screening approaches, the selection is not
usually between systems that are
brief or lengthy. The choice is usually between (1) a
system that is brief and comfortable
to the clinician and inoffensive to the patient or
(2) a complete absence of
any sex-related screening questions whatsoever.
There is no universally applicable
sexscreening
formula. Several approaches can be used.
|
The older style sex-screening
approach used to be: “How’s your sex life?” While this
fulfilled the wide spectrum and
brevity criteria, it was also nebulous and indefinite.
Being so general, it usually
elicited an equally vague answer (“fine”), which was undoubtedly
inaccurate on many occasions. In
addition, the question potentially covered the
whole of a patient’s current
sexual experience rather than concentrating
on what was problematic and
required attention.
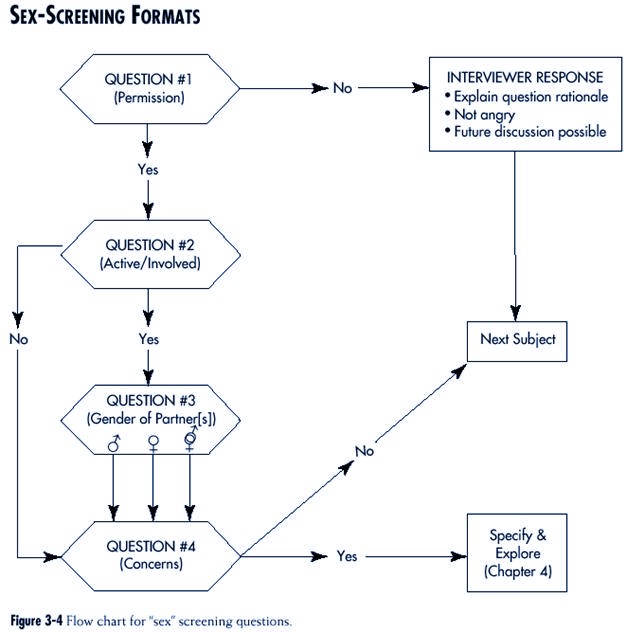
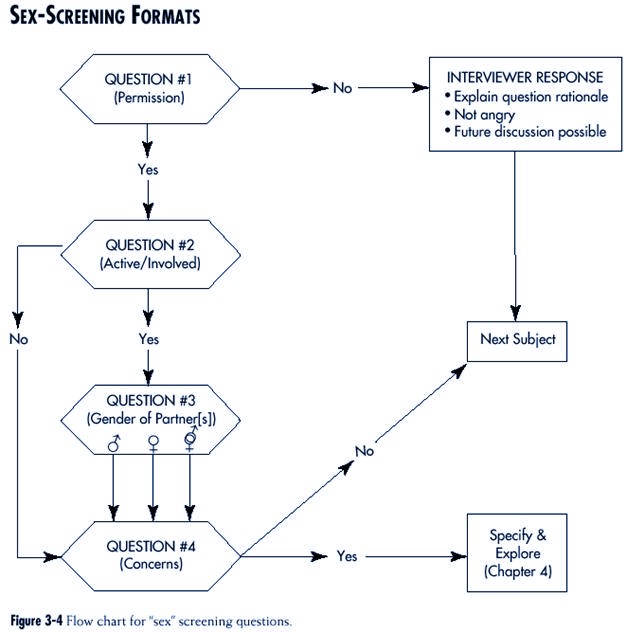
A preferred approach (Figure
3-4 and Box 3-2) begins with the question:
“CAN I ASK YOU A FEW QUESTIONS
ABOUT SEXUAL MATTERS?”
This is not really a “sex”
question but rather preliminary to other questions that
might follow. Use of the
permission technique was discussed in Chapter 2.
The answer to a permission question
is usually “yes.” After consent
is given, the interviewer
naturally continues to the next question. However,
in the unusual situation that the
patient says “no,” the interviewer
The answer to a permission question is
usually “yes.” After consent is given, the
interviewer naturally continues to the
next question. However, in the unusual
situation that the patients says “no,” the
interviewer has no ethical alternative
but to respect the patient’s decision and
continue to the next subject.
|
has no ethical alternative but to
respect the patient’s decision and continue to the next
subject. Before proceeding, some
of the implicit issues mentioned above should be
made explicit. In particular, the
interviewer should explain the rationale for asking the
question in the first place.
Reasons given may include the following:
• That this area is legitimate
for discussion in a medical setting even if
unconventional from the patient’s
point of view
• That the interviewer’s response
is one of understanding rather than
anger
• That the patient is free to
raise the topic at any time in the future
The second screening question
asks the patient: “ARE YOU SEXUALLY ACTIVE?”
This question is common
especially in relation to HIV/AIDS prevention. The question
could be made sharper if a time
frame is added. For example, it might be phrased:
“HAVE YOU BEEN SEXUALLY ACTIVE IN
THE LAST SIX MONTHS?” This
revision might be useful
particularly in situations where sexual activity may be regular
but not necessarily frequent, as for
example, in the elderly.
The meaning of the phrase
“sexually active” could be more specific if it included
some definition of the word
“active.” “Active” might refer to actions with a partner,
with oneself (masturbation), or
both. If a patient has a partner, couple sexual activities
should be the focus of this
question, so that the question might be: “HAVE YOU
BEEN SEXUALLY ACTIVE WITH A
PARTNER IN THE PAST SIX MONTHS?”
If the patient does not have a
sexual partner, the definition of “active” might logically
include solo sexual experiences.
However, since the subject of masturbation is often a
sensitive one for patients and
clinicians and, since it is infrequently reported as a problem
with sexual function or practice,
one might reasonably refrain from asking about
this specific subject in the
context of screening questions.
There are two potential problems
with the word “active”:
• Teenagers may not understand
what the word encompasses. Talking
with teenagers may be one
instance in which the word “sex” is useful,
since teens (unlike adults) often
have a broader definition than simply
intercourse. In using this
approach, the health professional must clarify
what practices are entailed
within the word “sex.”
• Some people interpret the word
“active” concretely and consider themselves
“passive,” so that even if
sexually involved with another person
they might answer the question in
the negative. It might be better to
Box 3-2
Sex Screening Questions
1. Can I ask you a few questions about
sexual matters?
2. Have you been sexually active with a
partner in the past six months?
3. With women? men? both?
4. Do you or your partner have any sexual
concerns?
|
use the word “involved” instead
of “active” in such situations. (A strong
counter argument is that the word
“active” has become part of the English
lexicon and that professionals
and adult patients are adjusted to
its use.)
The final version of the second
sex-screening question might therefore be: “HAVE
YOU BEEN SEXUALLY ACTIVE (OR
INVOLVED) WITH A PARTNER IN THE
PAST SIX MONTHS?”
A “yes” answer to the question of
sexual activity results naturally in the interviewer
proceeding to the next item,
which may be about the gender of the partner—opposite
or same sex. (Questions are
formulated by using the words, “men” and “women,” rather
than “opposite” and “same”[see
immediately below].) Acquiring information about sexual
orientation is vital for reasons
outlined in Chapter 7 (see “Sexual Orientation: Issues
and Questions”).
The third sex-screening question
is actually an extension of the second and attempts
to determine with whom the
patient has been sexually active. The question is asked
only if the patient says “yes” to
the second question and can be phrased (e.g., when
talking with a man): “HAVE YOU
BEEN SEXUALLY ACTIVE WITH WOMEN,
OTHER MEN, OR WITH BOTH?”
Following a “no” answer to the
question of whether or not a patient is sexually
active, an attempt should be made
to discover whether or not the person’s inactivity
is a concern. If it is, this
requires some exploration by the interviewer and an explanation
from the patient. This, in turn,
leads into a diagnostic process. If sexual
inactivity is not a concern, the
interviewer could naturally proceed to the fourth
and last screening question,
which is: “DO YOU OR YOUR PARTNER HAVE
ANY SEXUAL CONCERNS?”
The utility of a question about
“concerns” lies in the fact that it is open-ended and
problem-oriented. However, one
problem with this question is its subjectivity. A more
direct, objective, and still open-ended
and problem-oriented version would be, “DO
YOU OR YOUR PARTNER HAVE ANY
SEXUAL DIFFICULTIES?” A third possibility
is the same question but with
some added specific examples. The question
could then become: “(for a
man) DO YOU OR YOUR PARTNER HAVE ANY
SEXUAL DIFFICULTIES, SUCH AS WITH
YOUR INTEREST LEVEL, ERECTIONS,
OR EJACULATION?” (For a woman) “.
. . SUCH AS WITH YOUR
INTEREST LEVEL, VAGINAL
LUBRICATION, ORGASMS, OR INTERCOURSE
PAIN?” These
examples are of sexual dysfunctions. A clinician could, if desired, substitute
other examples such as STDs.
Any of these four questions
should fulfill the four criteria for screening questions
described above. If the screening
professional can ask only one question, the fourth is the
most desirable.
Conclusion
A screening system for “sex”
questions is a necessity for health professionals. The
arrangement must be comprehensive
(encompassing problems with sexual function
and sexual practices), the
questions few in number, and the problems sufficiently severe
and treatable. Practicality also
helps. There is not much use in proposing a system that
no one will use.
Screening questions about sexual
issues are a vital part of the health professional’s
intake procedure. However,
screening questions cannot be definitive. The question
inevitably arises: “What do you
do if you get a positive answer?” One does, of course,
the same as one would do with any
other subject. In the practice of a health professional,
this means allowing the patient
to talk and ask more questions as part of a
diagnostic process. This, in
turn, leads to a conclusion and to a treatment plan. The
next chapter discusses the first
of these two steps.
REFERENCES
1. Tiefer L: Sex is not a natural act and
other essays, Boulder, 1995, Westview Press.
2. Diagnostic and statistical manual of
mental disorders, ed 4, Washington, 1994, American
Psychiatric Association.
3. Masters WH, Johnson VE: Human sexual
inadequacy, Boston, 1970, Little, Brown and
Company.
4. Kaplan HS: Disorders of sexual desire, New
York, 1979, Brunner/Mazel, Inc.
5. Rosen RC, Beck JG: Patterns of sexual
arousal: psychophysiological processes and clinical
applications, New
York, 1988, The Guilford Press, pp 42-43.
6. Frank E, Anderson C, Rubenstein D:
Frequency of sexual dysfunction in normal couples,
N Engl J Med 299:111-115,
1978.
7. Ende JE, Rockwell S, Glasgow M: The sexual
history in general medicine practice, Arch
Intern Med 144:558-561,
1984.
8. Moore JT, Goldstein Y: Sexual problems
among family medicine patients, J Fam Prac
10:243-247,1980.
9. Garde K, Lunde I: Female sexual behaviour.
A study in a random sample of 40-year old
women, Maturitas 2:225-240, 1980.
10. Munjak DJ, Oziel LJ: Sexual medicine
and counseling in office practice: a comprehensive treatment
guide, Boston,
1980, Little, Brown and Company, pp 3-10.
11. Kolodny RC, Masters WH, Johnson VJ: Textbook
of sexual medicine, Boston, 1979, Little,
Brown and Company, pp 587-588.
12. Freund K: Screening in primary care for
women. In Carr PL, Freund KM, Somani S
(editors): The medical care of women, Philadelphia,
1885, W.B. Saunders Company, pp 1-13.
13. Hawton K: Sex therapy: a practical
guide. New York, 1985, Oxford University Press.
14. Browne A, Finkelhor D: Impact of child
sexual abuse: a review of the research, Psychol
Bull 99:66-77, 1986.