CHAPTER 1
Talking About Sexual Issues:
History-Taking and Interviewing
Significant obstacles exist between
the clinician’s capacity to ask a question and the patient’s capacity to
respond. Whereas comprehensive
knowledge is required of the cardiovascular system to cover all the
symptom bases, these questions
are typically asked without anxiety or inhibition once the questions are
memorized and their rationale
understood. Similarly, the patient experiences little or no hesitancy in
responding truthfully to these
paths of inquiry. The same milieu does not generally exist with sexual history
taking.
Green,
19791
Other than
descriptions of interviewing methods used by researchers2
and opinions
of specialist-clinicians who
treat people with sexual difficulties,3 health
professionals
have little guidance on the
subject of talking to patients about sexual issues. Less
still is any direction given to
primary care clinicians for integrating this topic into their
practices. For guidance on
sex-related interviewing specifically, the primary care clinician
may want to begin by examining
clinical research in the general area of interviewing,
as well as the observations of
those who have written about their personal general
interviewing ideas and practices.4
Some Research
on General Aspects of Health-related
Interviewing and History-Taking
As Rutter and Cox stated, “many
practitioners have advocated a variety of approaches
and methods on the basis of their
personal experience and preferences. . . [but]. . .
there has been surprisingly
little systematic study of . . .interviewing techniques for
clinical assessment purposes.”5
Only a few items from the research literature in the area
of health-related interviewing
are described here.
Direct Clinical Feedback
One interviewing-research
question has been the value of direct clinical supervision in
the development of interviewing
skills generally. While this form of supervision makes
sense intuitively, the process
has been subject to little research. One study compared
the value of direct clinical
feedback to medical students using four different techniques:
three of them (audio replay,
video replay, and discussion of rating forms) were
compared to a fourth whereby a
student interviewed a patient and subsequently discussed
findings (indirectly) with a
supervisor.6 The students who received any of the
three direct clinical
feedback methods did much better. The same individuals were
assessed five years later as
physicians and strikingly (since long-term follow-up studies
in health education are quite
unusual) those who received feedback “maintained their
superiority in the skills
associated with accurate diagnosis.”7
In another study, two groups of
medical students were videotaped on three different
occasions during the school year
while performing a history and physical examination.
8 Both groups viewed their
own tapes but one group received additional evaluative
comments by a faculty member. By
the end of the year, those in the latter group performed
significantly better in the
following:
• Their interviewing verbal
performance
• The content of the medical
history they obtained
• Their use of physical
examination skills
Teaching Interviewing Skills
One might conclude from the
findings of both studies that if direct supervision
proved superior in the process of
learning interviewing skills generally, the same conclusion
might be drawn for interviewing a
patient about a specific subject such as
“sex.” The importance of this
conclusion can not be exaggerated when one considers
the dearth of questions about
sexual issues in ordinary health histories. One way to
change this situation is to
deliberately teach the skill of sex history-taking and interviewing
in health professional schools
instead of (as now often seems to be the case)
seemingly expecting clinicians to
absorb this skill in the course of developing their
clinical practices.
It may be instructive to also
consider a series of studies of interviewing styles that
were based on talks with mothers
who were taking their children to a child psychiatry
clinic.5,9-14 These
interviews were conducted by experienced health professionals. Four
experimental interviewing styles
were compared for their efficacy in eliciting factual
information and feelings. The
four were given the following names:
• Sounding board
• Active psychotherapy
• Structured
• Systematic exploratory
The research group concluded that
good-quality factual information required detailed
questioning and probing, that
several approaches were successful in eliciting feelings,
and that these two issues were
compatible in the sense that attending to one
did not detract from the other.
Although their findings were related more to the
process of interviewing and not
specific to any particular topic, their conclusions
seemed as applicable to the area
of “sex” as with any other. The clinically apparent
need for the health professional
to initiate sex-related questions when talking with
patients (see “Interviewer
Initiative” in Chapter 2) echoes the conclusion of these
studies that asking detailed
questions is more productive. In extrapolating from
these studies and insofar as
“sex” can legitimately be seen as psychosomatic, there
should be no incompatibility in
the attention that a clinician might give to the
acquisition of information that
is factual and related to feelings when talking to a
patient about sexual matters.15
Another study that examined the
proficiency in history-taking generally in secondyear
medical students also may have
implications for sex history-taking.16 Two
methods
of measurement were used:
• The Objective Structured
Clinical Examination (OSCE)
• A written test
The authors believed that patient
information could be divided into three domains:
1. Information required to make a
diagnosis
2. Information to determine risk
for future disease
3. Information to assess the
patient’s available support system
The study found that students
concentrated on obtaining diagnostic information on
both of the tests used and that,
unless modeled by faculty, information on risk factors
and psychosocial data was
omitted. Since sex-related problems are often relegated to
the psychosocial arena, an
assumption that one might derive from this study is that
unless a sexual problem is given
by the patient as a chief complaint (and therefore in
the “diagnostic” arena) it is
unlikely to be detected—unless faculty modeling occurs.
Extrapolations from all of these
studies in interviewing and historytaking
as far as “sex” is concerned
imply the following:
1. Teaching of skills by direct
supervision should be included in
health science educational
programs
2. Direct questions are more
productive
3. There is no difficulty in
attending to factual information and
feelings
4. Faculty modeling is a
significant element in the learning process
Integrating Sex-related Questions into a General
Health History
Texts on general aspects of health-related
history-taking and interviewing
reveal great inconsistency in the
definition of a “sexual history” and consequently
in what is expected of the health
professional. Some texts contain little or no information
on the subject17;
others include a separate chapter 1,18-22 or
portion of a chapter.
4,23 Complete
or partial chapters are usually brief and the information is so concentrated
that the content is difficult to
use in a practical sense. Some authors focus on
“sex” as it relates to a particular
psychiatric or medical disorder, for example:
1. Sexual desire in depression24
2. Sexual abuse as it relates to
dissociation, posttraumatic stress disorder, and somatization
disorder25
3. The “hysterical” patient26
4. Sexually transmitted diseases27
Others focus special attention on
a particular sexual problem.21 Some
authors recommend
asking about the patient’s past
sexual development28; others suggest a focus
on
current problems.20
Specific suggested questions are offered by some,19
and others may
Extrapolations from studies in interviewing
and sex history taking imply:
1. Teaching of skills by direct supervision
should be included in health science
educational programs
2. Direct questions are more productive
3. There is no difficulty in attending to
factual information and feelings
4. Faculty modeling is a significant
element
in the learning process
|
also include a brief rationale
for these questions.29 When questions are
suggested, little
guidance is usually given on when
they should be asked.
“Human Sexuality” textbooks are
also of limited help. Some may include a chapter
on “assessment” or “sex”
history-taking and interviewing.30-32 Although
the quality of
information in these chapters may
be high, the amount that is squeezed into this one
section results in “information
overload” and therefore becomes of minimal practical
use to the frontline clinician.
Journal articles on sex
history-taking provide a similar variety of opinions about
what should be included. The
advent of HIV/AIDS has pushed physicians into promoting
the need for taking a sex
history.33,34 So, too, is the effect on health
professionals
of the recognition of the
frequency of child sexual abuse in the history of adults.35
Sometimes, history-taking
suggestions are in the form of topics to be covered rather
than specific questions to be
asked.36
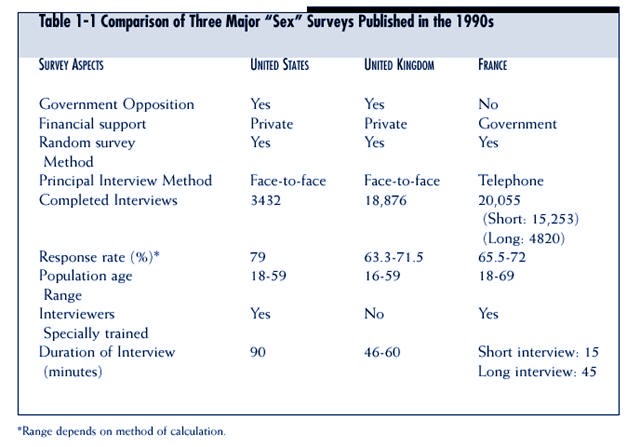
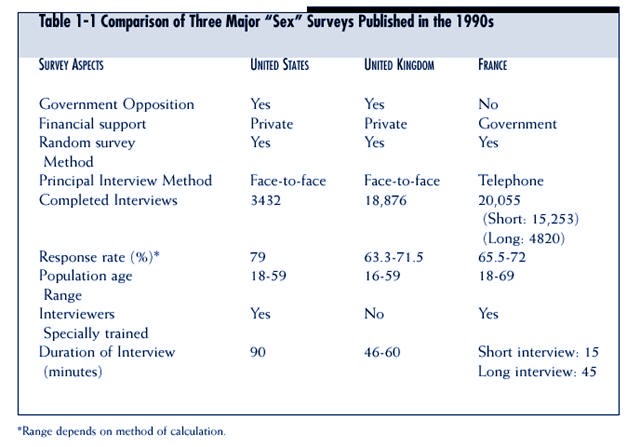
Among the more informative
sources of information on sex-related interviewing
and history-taking (but still of
limited value to primary care clinicians) are the comments
about interviewing that are
attached to some of the community based research
reports on sexual behavior.
Kinsey and his colleagues included a chapter on the subject
of interviewing in their volume Sexual
Behavior in the Human Male.37 More
recently, largescale
“sex” surveys in the United
States38 (see introduction to PART I), the United
Kingdom,39 and
France40 included reports about the interviewing
process when outlining
their study design (see Table 1-1
for a comparison of some aspects of the three
surveys).
Thus health-related interviewing
texts, specialty books on “Human Sexuality,” and
journal articles are enormously
variable in their content when considering sex historytaking
and tend to be disappointing in
that they provide little aid to clinicians.
Studies in Medical
Education That Relate to General Aspects
of Sex History-taking
In the 1960s and 1970s, sex
education in medical schools concentrated on providing
information about “sex” and
helping people to be more at ease with the subject.
Beginning in the 1980s, some
schools added a focus on skills, that is, interviewing
and history-taking, or, to put it
differently, they added focus on the
practical issue of how physicians
and patients actually talk about the subject of
sex. Attitudes and practices of
sex history-taking have been examined from a
research viewpoint, and
understanding conclusions from these studies may provide
some practical direction.
Comfort and Preparedness
Comfort and preparedness in
“taking a sexual history” was studied in a group of
first-year medical students.41,42
The idea of including this topic in a medical history,
as well as facilitating factors
and obstacles, was examined. The authors found
that the sexual orientation of
the patient seemed an important variable in that
students expected to be most
comfortable with heterosexual patients of the same
sex and least comfortable with an
(presumably gay) AIDS patient. The authors
also found that “the most
consistent predictor of both knowledge and attitudes
about sexual history-taking was a
student’s personal sexual experience.” The kinds
of experiences that were
particularly linked with comfort and preparedness in taking
a sexual history were:
1. Having taken a sexual history
in the past
2. Having spoken to a health
professional oneself about a sexual concern
3. Having a homosexual friend
Age seemed related only to the
extent that older students expected to be more comfortable
with an AIDS patient.
Practice
The importance of practice was
seen in a study of medical students who were involved
in different sexuality curricula
at two different schools.43 In one,
students were not
expected to be involved in sex
history-taking. In the other, students conducted a sex
history with a volunteer or
observed one taking place. The curricula were otherwise
similar. The three groups (no
interview, conducting an interview, and observing an
interview) were assessed
regarding knowledge about:
• Sexual issues
• The propriety of including
sex-related information in a medical history
• Self-confidence in the ability
to conduct the interview
The students who previously
conducted a sex-related interview did significantly better
than those who were neither
participants nor observers. However, findings relating to
students who were in the observer
group were intermediate on measures of knowledge
and perceived personal skill.
The reasons, “why other doctors
fail to take adequate sex histories,” were determined
in another study44
and include the following:
1. Embarrassment of the
physicians
2. A belief that the sex history
is not relevant to the patient’s chief
complaint
3. Belief that they (the
subjects) were not adequately trained
A large majority of senior
medical students thought that knowledge by
a physician of a patient’s sexual
practices was an important part of the
medical history but only half
were confident in their ability to actually
acquire this information from a
patient.
Social and Cultural Factors
Social and cultural factors
relating to the patient also seem to influence whether or not
a sex history is taken. Sixty
emergency room medical records of adolescent girls who
complained of abdominal pain that
required hospitalization were reviewed.45 The
authors found that asking about
sexual issues in the context of an emergency room
occurred a great deal more with
individuals from minority groups than with white
adolescents with the same
complaint. They concluded that racial stereotyping was an
important factor in asking
questions about sexual experiences. Although they supported
the inclusion of such questions
in an assessment, the authors argued that histories
in an emergency room should be
characterized by efficiency and a minimum of
irrelevant questioning, and that,
in spite of the pertinence of questions about sexual
experiences to the complaint of
abdominal pain in an adolescent girl, such questions
were more often omitted in those
who were white.
Skills Versus Self-awareness
In a demonstration of the sex
history-taking usefulness of direct teaching of skills compared
to sexual self-awareness, family
practice residents were randomly allocated to
two groups emphasizing one or the
other of these approaches.46 Each
group received
two hours of training. The first
hour was common to both groups and involved general
counseling skills and information
about sexual dysfunctions. In the second hour, the
two groups were separated and
concentrated on sexual history-taking issues or the
comfort and sexual self-awareness
of the resident. One week later, residents conducted
a videotaped interview with a
simulated “patient” with sexual and other problems but
who was also instructed to reveal
sex-related information only if asked directly. Almost
all subjects (11/12) in the
skills-oriented group asked the “patient” about the nature of
her sexual difficulty, compared
to 25% (3/12) of the awareness-oriented group.
Clinical Practice
A large majority of senior medical students
thought that knowledge by a physician
of a patient’s sexual practices was
an important part of the medical history
but only half were confident in their
ability to actually acquire this information
from a patient.
Physicians in clinical practice
(versus medical students and residents in educational
programs) also have been studied.
In a widely quoted and well-conceived study, a
group of primary care internists
were taught to ask a set of specific sex-related questions
of all new patients attending an
out-patient clinic.47 These physicians were then
compared to nontrained
colleagues. After the visit, physicians completed a questionnaire
and patients were interviewed
concerning their encounter with the physician.
The following results were
noteworthy and instructive:
1. More than half of the patients
had one or more sexual problems or areas of
concern
2. Age and sex did not influence
the prevalence of sexual problems
3. Many more patients (82%) who
saw trained physicians were asked about sexual
functioning than those who saw
untrained physicians (32%)
4. Among both groups of
physicians, discussions about sexual issues were more
likely if the patient was less
than 44 years old
5. Ninety one percent of the
entire group of patients thought that a discussion
about sexual issues was, or would
be, appropriate in a medical context and
approval was almost unanimous
(98%) among patients whose physician had, in
fact, included a sex history
6. Age of the patient was not a
factor in the determination of appropriateness
7. Thirty eight percent of the
entire patient group thought that follow-up for sexual
problems would be helpful
8. Physicians found that, in many
instances, the sex history was helpful in ways
other than simply as a means to
identify sexual problems or concerns
In summary, medical students,
family practice residents, and physicians in clinical
practice in the community have all
been studied on the issue of sex history-taking. The
following factors appear to
influence the learning process:
1. Having talked to patients
about sexual issues in the past
2. Having a sexual problem
oneself and having discussed it with a health
professional
3. The sexual orientation of the
patient
4. Having a homosexual friend
5. The belief that asking about
sexual issues is relevant to the patient’s concerns
6. Having received specific
training
7. Social and cultural issues
Studies in Medical
Education on Sex History-taking
in Relation to HIV/AIDS
There is little question that
HIV/AIDS is the major impetus for the recent teaching
of sex history-taking in medical
schools and the promotion of sex history-taking
among practicing physicians. This
development results from the knowledge that sexual
activity represents the prime
method of viral transmission. Many agree with the
statement “that the taking of a
candid and nonjudgmental sexual history is the cornerstone
of HIV preventive education. . .”48
Recognition of the crucial position of
physicians in HIV prevention has
resulted in several studies of physician
sex history-taking practices.
In general, studies of physicians
with different levels of medical
education and experience (e.g.,
internal medicine residents, primary
care clinicians) and using
various research techniques (e.g., standardized
patients, telephone interviews)
indicate the infrequency and/or
inadequacy of history-taking
around vulnerability to HIV/AIDS
infection and the consequent
inability to take preventive measures.
48,49-52 One of
these surveys demonstrated that in spite of the finding that
68% of 768 respondents said they
had received “human sexuality training” in medical
school, only a small minority of
primary care physicians routinely screened
patients for high-risk sexual
behavior.51 “Sexuality Training” was evidently helpful
after the fact,
since physicians who received this training in their medical education
“felt more comfortable in caring
for patients known to be infected. . .” with HIV.
Another study showed that while
self-reports of questions concerning homosexuality
doubled and questions about the
number of sexual partners tripled, questions
concerning sexual practices
increased by only 50% over the five years of
the project (1984-89).53
Yet another study demonstrated that only 35% of primary
care physicians reported that
they routinely (100%) or often (75%) took a
sex history from their patients.
Less than 20% of those who took histories
reported asking questions regarding
sexual activities that increase the risk of
acquiring HIV/AIDS.54
Two particularly revealing
projects involved a visit to primary care clinicians by a
simulated patient. In the first
study, physicians agreed to participate after being told
that a simulated patient would
appear in their practice.55 The
“patient” was female in
order to include
obstetrician-gynecologists. Other than obtaining prior agreement, the
“patient” was unannounced. She
revealed the following information:
• That she had been exposed to Chlamydia
by a previous partner
• She expressed interest in
engaging in sexual activities with a new partner
• She wanted to talk about
concerns regarding STDs generally and HIV
in particular
Comparisons were subsequently
made between the report of the “patient” and the selfreport
of the physician on several
issues, including risk assessment and counseling
recommendations. The greatest
discrepancies (all of which involved physicians overestimating
their history-taking skills in
the opinion of the “patient”) occurred with the
following topics:
• STD history
• Patient use of IV drugs
• Patient sexual orientation
• Condom use
• Counseling concerning anal
intercourse and use of a condom
• Safe alternatives to
intercourse
In spite of the finding that 68% of 768
respondents said they received “human
sexuality training” in medical school,
only a small minority of primary care
physicians routinely screened patients
for high-risk sexual behavior.
|
In the second simulated-patient
study, the “patient” had a history of engaging in
sexual activities that made her
vulnerable to HIV/AIDS infection.56 Physicians
were
provided with educational
materials before the visit. Whether these
materials were used or not did
not alter the finding that the questions
least frequently asked of the
“patient” were about oral or anal sex practices,
sexual orientation, and the use
of condoms. The authors concluded
that there was a need for
prevention training.
From these HIV/AIDS-related
studies, one might conclude that the
generic form of “Human Sexuality”
training in medical schools seems
to result in greater acceptance
toward those who already have HIV/
AIDS but it is insufficient in preventing
transmission. Effective preventive
behavior by physicians evidently
requires more specific curricular intervention
that addresses history-taking
skills and, in particular, inquiry
about patient sexual practices.
What, Then
, Is the Definition of a Sex (or Sexual) History?
Is taking a sex history by a
family physician who has only a few minutes to ask questions
about sexual issues and wants to
concentrate on, for example, STDs and HIV/
AIDS-related sexual behavior the
same as for a forensic psychiatrist who is evaluating
a patient referred because of
pedophilia? Is it the same (in time and content) for a
health professional asking
questions about child sexual abuse as for an interviewer
involved in a population survey
in which each interview might take hours to complete?
Is it the same for a clinical
psychologist or psychiatrist who asks a few screening questions
as part of the assessment of a
patient who is depressed as it is for a clinical sexologist
who is evaluating a couple
referred specifically because of erectile problems?
The answer to these questions is
obviously “no.” In all these situations, the result
might be called a “sex history”
but the time involved and the questions asked would be
quite different. Rather than use
the singular, it might be more reasonable to talk in the
plural, that is, of sex
histories—inquiries that are sexual in nature but differ because of
the diverse requirements of the
situations. In fact, instead of considering
a “sex history” or “sex
histories,” it may be easier to simply think
about the task of talking to a
patient about sexual matters.
A primary care clinician must
therefore be skilled in talking to
patients about a variety of
sexual issues, depending, among other
things, on the patient, the
problem presented, the amount of time
available for questioning, and
the context in which the patient is
seen.
Practical Aspects
of Introducing Sexual Questions
Into a Health-related
History
Practical aspects of talking to
patients about sexual matters can be viewed in the context
of the familiar format of why,
who, where, when, how, and what. This conceptual
The generic form of “Human Sexuality”
training in medical schools seems to
result in greater acceptance toward
those who already have HIV/AIDS but it
is insufficient in preventing transmission.
Effective preventive behavior by physicians
evidently requires more specific
curricular intervention that addresses
history-taking skills and, in particular,
inquiry about patient sexual practices.
Instead of considering a sex history or
sex histories, it may be easier to simply
think about the task of talking to a
patient about sexual matters
|
arrangement has been used
elsewhere in dissecting this subject but the content here is
different.1
So is the order. Issues that involve the manner in which questions
are
phrased (how) are considered in
Chapter 2, and which questions to ask (what) are
discussed in Chapters 3, 4, and
5.
Why
Discussion May Not Occur
(Box 1-1)
The following may be reasons why
discussions of sexual topics in a
health care setting do not occur:
1. Not knowing what to do with
the answers is the most common
reason given by physicians in
particular for avoiding the topic of
“sex” in medical history-taking.
When investigating what this explanation means,
two factors become evident:
• Uncertainty about what the next
question should be
• Perplexity regarding what to
offer the patient after all the questions are
asked and “Pandora’s box” is
opened
2. Worry that patients might be
offended by an inquiry into this area is a recurrent
theme of medical students. In
spite of the almost uninhibited media display of
sexuality, many people (including
medical students and physicians) continue to
regard sexual issues as
“personal” and are concerned that questions in this area
might be regarded as intrusive.
3. Lack of justification is a
common explanation given by medical students for the
frequent omission of sexual
topics from medical histories. However, when some
medical problems are presented to
a physician, specific aspects of a person’s
sexual life experience are often
the subjects of inquiry (e.g., issues that may be
medically relevant). Examples
include:
• Sexual dysfunctions associated
with diabetes mellitus57
• Sexual sequelae of child sexual
abuse35
Thus it seems as if an
association between “sex” and a medical disorder must be
demonstrated before
there is sufficient rationale to include sex-related questions in
a medical history. A closely
related issue is doubt among some health professionals
about the acceptability of sexual
issues in health care apart from disorders
that affect others (such as
STDs).
4. Talking with older patients
about sexual matters appears difficult for health
professional students. The age of
the student may be relevant, since many
are much younger than their
patients. The student may find that this situation
resembles talking with their
parents about the subject (an experience
that most would not have had and
that may be thought of as highly embarrassing
if it did occur). Avoidance of
discussing sexual issues with older
patients is particularly
unfortunate because some sexual difficulties clearly
become more common with
increasing age. For example, menopause in
women can result in discomfort
with intercourse, which, in turn, is explained
by decreased estrogen, resulting
in diminished vaginal lubrication.58 Menopausal
women will obviously not be well
served by the medical establish-
Not knowing what to do with the answer
is the most common reason given by
physicians for avoiding the topic of sex.
|
ment if they are not asked about
discomfort or pain with intercourse. Not
surprisingly, when women in
general are surveyed on the acceptability of
talking to a physician about
sexual concerns, almost three fourths think that
it is appropriate to do so.
Moreover, the response seems to be age related
in that approval increases with
age.59
5. Magnified concerns about
professional sexual misconduct and consequent licensure
problems result in reluctance by
some health professionals to initiate conversations
with patients about sexual
issues. The primary organization responsible
for medical malpractice insurance
in Canada has, in an exaggerated way,
cautioned their clients about
discussions with patients on the subject of sex and
has thereby magnified the already
difficult problem of health professional
restraint.60
6. The appropriateness of sex-related
questions in the acute stage of an illness may
be viewed by the health
professional as a dubious focus because of more pressing
patient concerns. An example is
when the patient has little opportunity for sexual
experiences with a partner (e.g.,
a situation that occurs when a patient is in
hospital). In this illustration,
sex is defined narrowly as related only to the function
of the genitalia.
7. Unfamiliarity with some sexual
practices (e.g., gay patients talking to a heterosexual
physician) may restrain the
health professional from introducing the
topic.
Why
Discussion Should Occur
(Box 1-2)
Reasons why discussions should
occur in a health care setting include the following:
1. HIV/AIDS, as everyone knows,
is a sexually transmitted disease that is also lethal.
It has become a powerful
(perhaps, the most convincing) stimulus for
sex history-taking by health
professionals (see introduction to Part I).61
Considering HIV/AIDS, prevention
is, at the moment, the best deterrent.
This, in turn, means talking to
patients about their sexual practices.
As used here, the term sexual
practices refers to:
• The types of sexual activities
engaged in by the patient, as well
Box 1-1
Why ‘Sex’ Questions Are Not Asked
1. Unclear what to do with the answers
2. Unfamiliarity with treatment approaches
2. • Uncertainty about the next question
2. Fear of offending patient
3. Lack of obvious justification
4. Generational obstacles
5. Fear of sexual misconduct charge
6. Sometimes perceived irrelevant
7. Unfamiliarity with some sexual practices
|
Considering HIV/AIDS, prevention is the
best deterrent. This means talking to
patients about their sexual practices.
|
as the nature of relationships
with sexual partners
• The characteristics of sexual partners
• The “toys” (mechanical
adjuncts such as vibrators) used in sexual
activities
• Methods used to prevent STD
transmission and conception
In the words of Hearst:
“Responsible primary care physicians
no longer have the option of
deciding whether to do AIDS
prevention; the question today is
how to do it. . . .”62 Health
professionals are simply not
fulfilling their role if inquiry is not
made about sexual practices, and
if, in the process, the opportunity for dispensing
preventive sexual advice is lost.
Physicians, in particular, are thought
to be in a unique position to
prevent HIV infection, since 70% of adults in the
United States visit a physician
at least once each year and 90% do so at least
once in five years.51
2. Many medical disorders such as
depression63 and diabetes57 are
known to disrupt
sexual function. A comprehensive
view of such disorders is plainly impossible
without also asking how a
patient’s sexual function is affected (see Chapter 8).
3. Treatments such as surgery64
or drugs65 can interrupt sexual function.
A health
professional should inquire about
drug side effects (see Chapter 8 and Appendix
III).
4. Inquiry into past sexual
events may be essential to understand the nature of a
disorder in the present. Such is
the case with lack of sexual desire after sexual
assault as an adult or child (See
Chapters 8 and 9).66
5. The observation that “. .
.sexual function is a lifelong capacity, not normally
diminished by middle or older
age” represents a change in social attitudes.67 The
aging of the population translates
into increasing expectations by many patients
regarding sexual function. These
hopes may conflict with the difficulty that
many young health professionals
experience in discussing sexual matters with
older people.
6. Sexual dysfunctions are common,
at least on an objective level.68 So, too,
are
sexual difficulties. Intuitively,
it seems reasonable for a health professional to ask
particularly about problems that
occur most frequently (sexual dysfunctions and
difficulties) as compared to
problems that are unusual.
7. On the topic of sex as well as
others, health professionals tend to be problem oriented.
This book and many others on the
same subject admittedly “focus on the
darker side. . .more than on its
brighter side”38 (p. 351). However, the “other side”
is what happens when “things go
right.” Laumann and colleagues (see introduction
to PART I) addressed this side of
sex in their chapter (brief by their own admission)
on the association between sex,
and health and happiness (pp.351-375).
Sexual activity and good health
are related. Of patients in the Laumann et al.
study who had no sexual partners
in the past 12 months, most (6% versus 2% of
the entire sample) were in poor
health.38 Sexual activity and happiness were
correlated.
Of those who considered
themselves “extremely or very happy” (compared
to those who were “generally
satisfied” or “unhappy”), three groups of
respondents were most prominent:
Physicians are thought to be in a unique
position to prevent HIV infection, since
70 percent of adults in the United States
visit a physician at least once each year
and 90% do so at least once in five
years
|
• Those who had one sexual
partner
• Those who had “sex” two to
three times per week
• Women who “always” or “usually”
experienced orgasm in partnered sex
(p. 358)
The association between “sex,”
emotional satisfaction, and physical pleasure was
examined also in the Laumann et
al. study38 (pp. 363-368). Those who found
their relationships “extremely or
very” pleasurable or satisfying were more often
the people who had one (versus
more than one) sex partner, especially if the
partner was a spouse or there was
a cohabitational relationship (p. 364). The
authors commented that while
“association is not causation (p. 364),” “the quality
of the sex is higher and the
skill in achieving satisfaction and pleasure is
greater when one’s limited
capacity to please is focused on one partner in the
context of a monogamous,
long-term partnership”(p. 365).
8. Why not? Masters and Johnson
asked this question (still germane more than 25
years later) in a medical journal
editorial that did not receive the attention that
it seemingly deserved.69
They were critical of the opinion that physicians apparently
needed special justification for
asking “sex” questions while paradoxically
being taught to ask questions
about everything else in the course of a general
medical examination. “The
biologic and behavioral professions must accept the
concept that sexual information
should be as integral a part of the routine medical
history as a discussion of bowel
or bladder function.”
9. Not including sexual matters
in a health history can sometimes be considered
negligent and possibly unethical.
An example is the second case history provided
in the introduction to PART I. In
that instance, the physician (in a “sin” of omission
rather than commission) clearly
failed the medical dictum of “do no
harm.”
Who (which patients) Should Be Asked About Sexual Issues?
Almost all patients should be
given the opportunity to talk about a sexual
concern in a health professional
setting. Providing such an opportunity
Box 1-2
Why Ask Questions About “Sex”?
1. Morbidity and mortality—STDs and
HIV/AIDS
2. Symptoms of illness
3. Treatment side effects
4. Past may explain present problems
5. Function potentially lifelong
6. Dysfunctions and difficulties are common
7. Association with health and happiness
8. Why not?
9. May be negligent if ignored
|
Almost all patients should be given the
opportunity to talk about a sexual concern
in a health professional setting.
|
does not mean asking a “sex”
question but rather using a method that involves asking if it’s
OK to ask a “sex” question (see
“Permission” in Chapter 2 and an example of a specific
permission question in Chapter
3).
Common sense dictates at least
two exceptions to routinely giving
everyone an opportunity to talk
about sexual issues. First, it obviously does not apply
to an emergency setting (unless,
for example, the emergency is sexual in nature, such
as sexual asphyxia [see Chapter 8
for definition]). Rather it applies to situations such
as the first few visits of an
“intake” procedure. Second, when applied to physicians, the
idea of routinely giving everyone
this opportunity relates more to generalists, that is,
primary care specialists (e.g.,
in medicine: family physicians, pediatricians, gynecologists,
and internists) and medical
specialists whose area of work is directly related to
sexual function (e.g.,
urologists). Providing an opportunity to talk about sexual issues
on a routine basis rather than a
selective basis does not apply to medical specialty areas
such as Ophthalmology and ENT
(ear, nose, and throat).
Where (in a health professional history) Should Questions
Be Asked About Sex?
Sometimes, a patient spontaneously
indicates that a sexual concern is the principal
reason for the visit. When this
occurs, the sexual problem obviously has priority. However,
such information usually has to
be elicited carefully. In a medical setting, three
different circumstances (not mutually
exclusive) exist in which this could happen:
1. The prime location in a
medical history for asking about sex-related information
is within a Review of Systems
(ROS [sometimes referred to as a
Functional Inquiry]; see
“Permission” in Chapter 2 for an example).
A ROS consists of a few questions
about each body system
to ensure that nothing is wrong
with a patient other than the
initial complaint(s). In such a
context, a few additional questions
about sexual concerns could be
easily included.
2. Another possibility for the
introduction of questions about sexual
issues is within a Personal and
Social History. For example, in the
process of asking about
relationships, one could ask about sexual
concerns.
3. A sex-related question could
be asked during a physical examination
(least desirable and an option
that is, obviously, unavailable
to nonphysicians). For example,
one could ask about genital function
in the process of examining
genitalia. In one sense, this situation
is easier for physicians, since
it seems that psychological
defenses of patients are
diminished when their clothes are off. However, the lowering
of defenses during a physical
examination can be hazardous to the patient
because questions about sexual
issues can be misinterpreted as a physician’s sexual
invitation and the patient’s
misconception could provoke a charge of sexual harassment
or misconduct. Although
sex-related questions during a physical examination
may represent a more efficient
use of professional time, the potential for
misunderstanding is sufficiently
great that this method should be avoided.
When Should Questions About Sex Be Asked?
The lowering of defenses during a physical
examination can be hazardous to the
patient because questions about sexual
issues can be misinterpreted as a sexual
invitation by the physician and the
patient’s misconception could provoke a
charge of sexual harassment or misconduct.
Although sex-related questions
during a physical examination may represent
a more efficient use of professional
time, the potential for misunderstanding
is sufficiently great that this
method should be avoided.
Green offered a clear and
sensible opinion on when questions should be asked
about sexual issues: “The optimal
time. . .is not when a patient’s initial visit has
been prompted by influenza,
otitis media and bronchitis. Nor is the appropriate
time the anniversary of the
physician-patient relationship. . .Delay in approaching
the topic communicates
discomfort. The effect when ‘the subject’ is finally broached
is comparable to the painfully
familiar scene of a father who initiates discussion of
the ‘facts of life’ with his son
on his 13th birthday.”1 Generally
speaking, the aphorism
of ‘the earlier the better’
should be applied. Screening questions (see Chapter
3) can be introduced after the
acute problem that initially led the patient to the
health professional has
disappeared or is under control.
If a problem is introduced in the
process of screening, more detailed diagnostically
oriented questions can be asked
on a subsequent occasion (see Chapter 4). The diagnostic
process may involve a physical
examination (see Chapter 6) and the use of
laboratory tests (see PART II).
Summary
Extrapolations from studies on
general aspects of health- related interviewing and history-
taking imply the following:
1. Concerning sexual issues,
teaching of skills by direct supervision and feedback
should be included in health
science educational programs
2. An interviewer can attend to
both factual information and feelings
3. Faculty modeling in obtaining
information about the patient’s psychosocial status
and risk factors is a significant
element in the learning process
When considering the integration
of sex-related questions into a general health history,
interviewing texts, books on
“Human Sexuality,” and journal articles appear to be
of limited practical help.
Studies in sex history-taking
have involved medical students, residents, and practicing
physicians. The studies can be
separated into ones that considered sex historytaking
in general and those that focused
on the specific subject of STDs. In the former
group, factors found to be
associated with positive attitudes toward sex history-taking
and conducting such a history
were:
1. Personal sexual experience
2. The belief that such questions
were relevant to the patient’s chief complaint
3. Feeling adequately trained
4. Confidence in taking a sex
history
5. Having previously taken a sex
history
6. Having spoken to a health
professional oneself about a sexual concern
7. Having a homosexual friend
8. Social and cultural factors
9. Skill training (as compared to
personal comfort and self-awareness)
Studies that focused on “sex”
history-taking as it applies to HIV/AIDS prevention
indicate that relevant questions
occur infrequently and inadequately. Previous “sexuality training”
appeared to
be helpful to physicians in caring for those already infected
with HIV but it was insufficient
in the process of preventing transmission, which, in
turn, required an inquiry into
the sexual practices of the patient.
Rather than attempting to define
a “sex” history (there are many such definitions),
it might be more productive to
simply talk about asking questions of patients about
sexual matters. One might
consider the introduction of such questions under the headings
of Who, What, When, Where, Why,
and How.
Reasons why “sex” history-taking
does not regularly occur include:
1. Not knowing what to do with
the answers
2. Concern that patients might
regard “sex” questions as intrusive
3. Lack of a sense of
justification
4. Difficulty in talking to older
patients about this subject
5. Concern about accusations of
sexual misconduct
6. The sense that such questions
are inappropriate in the context of other difficulties
manifested by the patient
7. Lack of familiarity with some
sexual practices
Reasons why “sex” questions should
occur in a health history include finding that:
1. Such questions provide an
opportunity to introduce HIV/AIDS prevention information
2. Disrupted sexual function may
be a symptom of a medical disorder or it may be
a side effect of its treatment
3. Past sexual history may help
explain the present
4. Sexual issues are important at
all stages of the life cycle
5. Sexual dysfunctions in
particular are quite common
6. Sexual function is related to
general health
7. There is no explanation for
not asking questions of a sexual nature
8. Not asking “sex” questions may
constitute negligence from a legal point of
view
The problem of who should be
asked questions about sexual issues can be resolved
by saying that almost everyone
should have the opportunity to talk about sexual concerns
if they so choose. Other than
situations in which a sexual problem is the main
issue that brought the patient to
the health professional, questions can be asked in the
context of a medical review of
systems (ROS) or a personal and social history. Physicians
may also ask questions during a
physical examination but caution should be
exercised because of the
possibility of misinterpretation of the intent and consequent
accusations of sexual misconduct.
It may be easier to say when the time to ask such
questions is not optimal than
when it is.
“Sex” questions are improper in
the midst of concern over some other issue that
brought the patient to the
attention of the health professional. (Questions about many
topics are reasonably omitted in
such situations). The context for “sex” questions is
after the acute problem subsides
and the professional is reviewing general aspects of
the patient’s health history.
The “how” (or methods used) of
asking “sex” questions is considered in detail in
Chapter 2 and is therefore not
included here. Similarly, the “what” (content) did not
form part of Chapter 1, since it
forms the content of Chapters 3, 4, and 5 and subsequent
portions of the book.
REFERENCES
1. Green R: Taking a sexual history. In Green
R (editor): Human sexuality: a health practitioner’s
text, ed 2,
Baltimore and London, 1979, Williams and Wilkins, pp 22-30.
2. Pomeroy WB, Flax CC, Wheeler CC: Taking
a sex history: interviewing and recording, New
York, 1982, The Free Press.
3. Risen CB: A guide to taking a sexual
history, Psychiatr Clin North Am 18(1):39-53, 1995.
4. Morrison J: The first interview: revised
for DSM-IV, New York, 1995, The Guilford Press.
5. Rutter M, Cox A: Psychiatric interviewing
techniques: 1. methods and measures, Br J
Psychiatry 138:273-282,
1981.
6. Maguire P et al: The value of feedback in
teaching interviewing skills to medical
students, Psychol Med 8:695- 704,
1978.
7. Maguire P, Fairbairn S, Fletcher C:
Consultation skills of young doctors: 1—benefits of
feedback training in interviewing as students
persist, Br Med J 292:1573-1576, 1986.
8. Stone H, Angevine M, Sivertson S: A model
for evaluating the history taking and
physical examination skills of medical
students, Med Teach 11:75-80, 1989.
9. Cox A, Holbrook D, Rutter M: Psychiatric
interviewing techniques VI. Experimental
study: eliciting feelings, Br J Psychiatry
139:144-152, 1981.
10. Hopkinson K, Cox A, Rutter M: Psychiatric
interviewing techniques III. Naturalistic
study: eliciting feelings, Br J Psychiatry
139:406-415, 1981.
11. Rutter M et al: Psychiatric interviewing
techniques IV. Experimental study: four
contrasting styles, Br J Psychiatry 138:456-465,
1981.
12. Cox A, Rutter M, Holbrook D: Psychiatric
interviewing techniques V. Experimental
study: eliciting factual information, Br J
Psychiatry 139:29-37, 1981.
13. Cox A, Holbrook D, Rutter M: Psychiatric
interviewing techniques VI. Experimental
study: eliciting feelings, Br J Psychiatry
139:144-152, 1981.
14. Cox A, Rutter M, Holbrook D: Psychiatric
interviewing techniques—a second
experimental study: eliciting feelings, Br
J Psychiatry 152:64-72, 1988.
15. Kaplan HS: Sex is psychosomatic
(editorial), J Sex Marital Ther 1:275-276, 1975.
16. Rezler AG, Woolliscroft JA, Kalishman SG:
What is missing from patient histories? Med
Teach 13:245-252,
1991.
17. Newell R: Interviewing skills for
nurses and other health care professionals, London, 1994,
Routledge.
18. Attarian P: The sexual history. In
Levinson D (editor): A guide to the clinical interview,
Philadelphia, 1987, W.B. Saunders Company, pp
226-234.
19. Long LG, Higgins PG, Brady D: Psychosocial
assessment: a pocket guide for data collection,
Norwalk, 1988, Appleton & Lange, pp
105-117.
20. Turnbull J: Interviewing the patient with
a sexual problem. In Leon RL: Psychiatric interviewing:
a primer,
ed 2, New York, 1989, Elsevier Science Publishing Co., Inc., pp 151-155.
21. Kraytman M: The complete patient
history, ed 2, New York, 1991, McGraw-Hill, pp 468-470.
22. Lloyd M, Bor R: Communication skills
for medicine, Edinburgh, 1996, Churchill Livingstone,
pp 73-84.
23. Coulehan JL, Block MR: The medical
interview: a primer for students of the art, ed 2, Philadelphia,
1992, F.A. Davis Company, pp 217-224.
24. Shea SC: Psychiatric interviewing:
the art of understanding, Philadelphia, 1988, W.B. Saunders
Company.
25. Othmer EO, Othmer SC: The clinical
interview using DSM-IV, vol 1, Fundamentals and vol 2,
The difficult patient,
Washington, 1994, American Psychiatric Press, Inc.
26. Mackinnon RA: The psychiatric
interview in clinical practice, Philadelphia, 1971, W.B. Saunders
Company, pp 115- 117.
27. Cohen-Cole SA: The medical interview:
the three-function approach, St. Louis, 1991, Mosby-Year
Book, Inc., p 82.
28. MacKinnon RA, Yudofsky SC: Principles
of the psychiatric evaluation, Philadelphia, 1991, J.B.
Lippincott Company, pp 53-54.
29. Aldrich CK: The medical interview:
gateway to the doctor- patient relationship, New York, 1993,
The Parthenon Publishing Group, pp 102-104.
30. Semmens JP, Semmens FJ: The sexual
history and physical examination. In Barnard MU,
Clancy BJ, Krantz KE (editors): Human
sexuality for health professionals, Philadelphia, 1978,
W.B. Saunders Company, pp 27-43.
31. Marcotte DB: Sexual history taking. In
Nadelson CC, Marcotte DB (editors): Treatment
interventions in human sexuality,
New York, 1983, Plenum Press, pp 1-9.
32. Hogan RM: Human sexuality: a
nursing perspective, ed 2, Norwalk, 1985, Appleton-Century-
Crofts, pp 161-173.
33. Lewis CE: Sexual practices: are
physicians addressing the issues? J Gen Intern Med 5(5
suppl):S78-81, 1990.
34. Gabel LL, Pearsol JA: Taking an effective
sexual and drug history: a first step in HIV/
AIDS prevention, J Fam Prac 37:185-187,
1993.
35. Wyatt G: Child sexual abuse and its
effects on sexual functioning, Annual Review of Sex
Research 2:249-266,
1991.
36. Alexander B: Taking the sexual history, Am
Fam Physician 23:147, 1981.
37. Kinsey AC, Pomeroy WB, Martin CE: Sexual
behavior in the human male, Philadelphia and
London, 1949, W.B. Saunders.
38. Laumann EO et al: The social
organization of sexuality: sexual practices in the United States,
Chicago, 1994, The University of Chicago
Press.
39. Johnson AM et al: Sexual attitudes and
lifestyles, Oxford, 1994, Blackwell Scientific
Publications.
40. Spira A, Bajos N, and the ACSF group: Sexual
behavior and AIDS, Brookfield, 1994, Ashgate
Publishing Company.
41. Vollmer SA, Wells KB: How comfortable do
first-year medical students expect to be
when taking sexual histories? Med Educ 22:418-425,
1988.
42. Vollmer SA, Wells KB: The preparedness of
freshman medical students for taking sexual
histories, Arch Sex Behav 18:167-177,
1989.
43. Vollmer SA et al: Improving the preparation
of preclinical students for taking sexual
histories, Acad Med 64:474-479, 1989.
44. Merrill JM, Laux LF, Thornby JI: Why
doctors have difficulty with sex histories, South
Med J 83:613-617,
1990.
45. Hunt AD, Litt IF, Loebner M: Obtaining a
sexual history from adolescent girls: a
preliminary report of the influence of age
and ethnicity, J Adolesc Health Care 9:52-54,
1988.
46. Liese BS et al: An experimental study of
two methods for teaching sexual history taking
skills, Fam Med 21:21-24, 1989.
47. Ende JE, Rockwell S, Glasgow M: The
sexual history in general medicine practice, Arch
Intern Med 144:558-561,
1984.
48. Calabrese LH et al: Physicians’
attitudes, beliefs, and practices regarding AIDS healthcare
promotion, Arch Intern Med 151:1157-1160,
1991.
49. Bresolin LB et al: Attitudes of U.S.
primary care physicians about HIV disease and AIDS,
AIDS Care 2:117-125,
1990.
50. Boekeloo BO et al: Frequency and
thoroughness of STD/HIV risk assessment by
physicians in a high-risk metropolitan area, Am
J Public Health 81:1645-1648,
1991.
51. Ferguson KJ, Stapleton JT, Helms CM:
Physicians’ effectiveness in assessing risk for
human immunodeficiency virus infections, Arch
Intern Med 151:561-564, 1991.
52. Curtis JR et al: Internal medicine
residents’ skills at identification of HIV-risk behavior
and HIV-related disease, Acad Med 69:S45-47,
1994.
53. Lewis CE, Montgomery K: The AIDS-related
experiences and practices of primary care
physicians in Los Angeles: 1984-89, Am J
Public Health 80:1511-1513, 1990.
54. McCance KL, Moser R Jr., Smith KR: A
survey of physicians’ knowledge and application
of AIDS prevention capabilities, Am J Prev
Med 7(3):141-145, 1991.
55. Russell NK et al: Extending the skills
measured with standardized patient examinations:
using unannounced simulated patients to
evaluate sexual risk assessment and risk
reduction skills of practicing physicians, Acad
Med 66 (Sept Suppl), S37-S39, 1991.
56. Bowman MA et al: The effect of
educational preparation on physician performance with
a sexually transmitted disease-simulated
patient, Arch Intern Med 152:1823-1828, 1992.
57. Schiavi RC et al: Diabetes mellitus and
male sexual function, Diabetologia 36:745-751,
1993.
58. Masters WH, Johnson VE: Human sexual
response, Boston, 1966, Little, Brown and
Company, p 240.
59. Maurice WL, Sheps SB, Schechter MT: Physician
sexual contact with patients: 2. A public survey
of women in British Columbia.
Paper presented at the meeting of the Society for Sex Therapy
and Research, New York, March 1995.
60. Information letter, Can Med
Protect Assoc 7:2, 1992.
61. Canadian AIDS Society. Safer sex
guidelines: health sexuality and HIV, Ottawa, 1994, Can AIDS
Society.
62. Hearst N: AIDS risk assessment in primary
care, J Am Board Fam Pract 7(1):44-48, 1994.
63. Nofzinger EA et al: Sexual function in
depressed men, Arch Gen Psychiatry 50:24-30, 1993.
64. Yavetz H et al: Retrograde ejaculation, Hum
Reprod 93:381-386, 1994.
65. Barnes TRE, Harvey CA: Psychiatric
drugs and sexuality. In Riley AJ, Peet M, Wilson C
(editors): Sexual pharmacology, New
York, 1993, Oxford University Press.
66. Becker JV et al: Level of postassault
sexual functioning in rape and incest victims, Arch Sex
Behav 15:37-49,
1986.
67. Tiefer L, Melman A: Comprehensive
evaluation of erectile dysfunction and medical
treatments. In Leiblum SR, Rosen RC
(editors): Principles and practice of sex therapy: update for
the 1990s,
ed 2, New York, 1989, The Guilford Press, p 208.
68. Frank E, Anderson C, Rubenstein D:
Frequency of sexual dysfunction in normal couples,
N Engl J Med 299:111-115,
1978.
69. Masters WH, Johnson VE: Undue distinction
of sex, N Engl J Med 281:1422-1423, 1969.